What Is Infertility?
According to the World Health Organization (WHO), infertility is defined as the inability to achieve pregnancy after 12 months or more of regular, unprotected sexual intercourse.
This can result from issues in either the male or female reproductive system—or sometimes both. In some cases, the cause of infertility remains unknown, a condition referred to as unexplained infertility. Regardless of the cause, identifying the underlying issue is a critical first step.
How is infertility diagnosed?
Infertility diagnosis involves a variety of tests and evaluations tailored to the individual. Your healthcare provider will consider your medical history, lifestyle, and sexual habits before recommending specific tests.
Male infertility diagnosis
Male fertility relies on the production of a sufficient number of healthy sperm by the testicles. These sperm must then be ejaculated into the vagina and travel through the reproductive tract to reach the egg for fertilization. Evaluating male infertility focuses on identifying and addressing any potential issues at these critical stages. Here’s an overview of the diagnostic steps and procedures involved:
Physical Examination
A comprehensive physical examination, including an evaluation of the genital area, is often the first step in diagnosing male infertility. This helps identify any visible abnormalities or conditions that may affect fertility.
Key Diagnostic Tests
- Semen Analysis: Your healthcare provider may request one or more semen samples for laboratory analysis. These samples are typically collected through masturbation or by interrupting intercourse to ejaculate into a sterile container. The lab evaluates sperm count, motility, morphology, and overall semen quality. In certain cases, urine tests may also be performed to check for the presence of sperm.
- Hormone Testing: Blood tests measure hormone levels, including testosterone and follicle-stimulating hormone (FSH), which regulate sperm production. If initial results indicate potential hormonal imbalances, further tests for luteinizing hormone (LH) and prolactin may be recommended. Measuring testosterone alongside other hormones provides a clearer picture of overall reproductive health.
- Genetic Testing: Genetic abnormalities can sometimes cause infertility. Testing may reveal inherited conditions or mutations affecting sperm production or function.
- Testicular Biopsy: In specific cases, a small tissue sample from the testicles may be examined under a microscope. This procedure is typically used to identify blockages or other conditions affecting sperm release. It may also help collect viable sperm for assisted reproductive techniques, such as in vitro fertilization (IVF).
- Imaging Tests: Ultrasound imaging can detect abnormalities in the scrotum, testicles, or glands involved in semen production. In rare cases, a brain MRI may be recommended to check for noncancerous tumors in the pituitary gland. These tumors can lead to excessive prolactin production, which may negatively impact sperm production.
- Advanced Semen Analysis: In rare instances, additional tests may be performed to assess sperm quality. For example, DNA fragmentation tests can identify genetic issues within the sperm that may affect fertility.
Comprehensive Approach to Diagnosis
Male infertility diagnosis often involves a combination of medical history review, physical examination, and laboratory tests. While not all men require every test, a tailored approach ensures that the underlying cause of infertility is accurately identified and addressed.
By diagnosing potential issues early, healthcare providers can recommend appropriate treatments, offering hope and solutions for individuals and couples navigating the challenges of infertility.
Women’s Infertility Diagnosis
A woman’s ability to conceive depends on the healthy release of eggs from the ovaries. The reproductive process involves the movement of an egg through the fallopian tubes, where it can be fertilized by sperm.
After fertilization, the egg must travel to the uterus and successfully implant into the uterine lining. Tests for female infertility aim to identify potential issues at any of these important stages. The assessment may include a physical examination, including a regular pelvic exam.
Diagnostic Tests for Female Infertility
- Ovulation Testing: This includes a blood test to evaluate hormone levels and determine if ovulation is occurring.
- Thyroid Function Test: If there are suspicions of thyroid gland problems contributing to infertility, a blood test is done to assess thyroid hormone production. Imbalances in thyroid hormone levels can affect fertility.
- Hysterosalpingography: This procedure examines the condition of the uterus and fallopian tubes, looking for blockages or other issues. A special dye is injected into the uterus, and X-rays are taken to visualize the reproductive structures.
- Ovarian Reserve Testing: This test helps the healthcare team assess the number of eggs available for ovulation. The process often begins with hormone testing early in the menstrual cycle.
- Hormone Tests: These tests focus on hormone levels that regulate ovulation and control various aspects of the reproductive process.
- Imaging Tests: Pelvic ultrasound is used to detect any uterine or ovarian abnormalities. Occasionally, a saline infusion sonogram, also known as a sonohysterogram, may be used to visualize detailed information within the uterus that may not be visible with a regular ultrasound.
Additional Testing
In rare cases, further testing may be necessary, including:
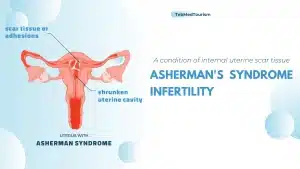
- Hysteroscopy: This procedure may be recommended based on specific symptoms. A thin, illuminated hysteroscope is inserted through the cervix into the uterus to examine for any irregularities. It can also assist in guiding minor surgical interventions.
- Laparoscopy: Laparoscopy involves making a small incision below the navel, through which a thin viewing device is inserted to examine the fallopian tubes, ovaries, and uterus. This procedure can identify conditions such as endometriosis, scarring, blockages, or other issues with the reproductive organs. Laparoscopy can also be used as a surgical method to treat certain conditions like fibroids or endometriosis tissue.
It’s important to note that not every individual undergoing infertility evaluation requires all of these tests. The selection of tests and their timing are determined through collaboration between you and your healthcare team. The goal is to identify the cause of infertility through a personalized diagnostic approach.
Conclusion
In summary, various diagnostic procedures and assessments are used to detect potential reproductive system issues.
For men, these include semen analysis, hormone testing, genetic testing, and imaging, while women undergo tests such as ovulation testing, thyroid function testing, hysterosalpingography, ovarian reserve testing, hormone tests, and imaging. Not all tests are necessary for every individual, and a personalized approach is taken in consultation with healthcare providers.
Despite the discomfort and expense associated with these tests, they are crucial in comprehending and addressing infertility. It’s also important to recognize that infertility is a complex issue, and even after extensive testing and counseling, there is no guarantee of achieving pregnancy.
However, these tests provide hope and guidance for individuals and couples as they navigate the challenges of infertility and explore assisted reproductive techniques.