Azoospermia is a medical term for zero sperm count in the ejaculate. It can be either “obstructive,” meaning that sperm cannot enter the ejaculate, or “nonobstructive,” meaning that the testis is not producing sperm as many as necessary.
When you have azoospermia, your ejaculate is devoid of sperm. An obstruction along the reproductive canal, hormonal abnormalities, problems with ejaculation, or problems with the anatomy or function of the testicles are some of its causes. There are numerous treatable causes. It might be feasible to recover live sperm for use in IVF and other assisted reproductive methods for other reasons.
What is azoospermia?
Azoospermia is a condition in which your ejaculate (semen) contains no sperm count and is one of the causes of infertility.
Testicles normally generate sperm. Your reproductive system contains sperm, which combine with fluids to make semen. The fluid that your penis discharges during ejaculation is called semen. Semen may be present in people with azoospermia, but it contains no sperm. Having “no sperm count” is another term for azoospermia.
Sperm count is something that some people have from birth, while others acquire as teenagers or adults. In some circumstances, azoospermia can be adequately treated with medication and surgery as part of infertility treatment in Iran. You are still able to have biological children despite having the disease.
About 1% of all men and 10% of infertile men suffer from non obstructive azoospermia. If 50,000 men attend a game in a stadium, between 5,000 and 7,500 of them will be infertile, and 500 of them will have azoospermia!
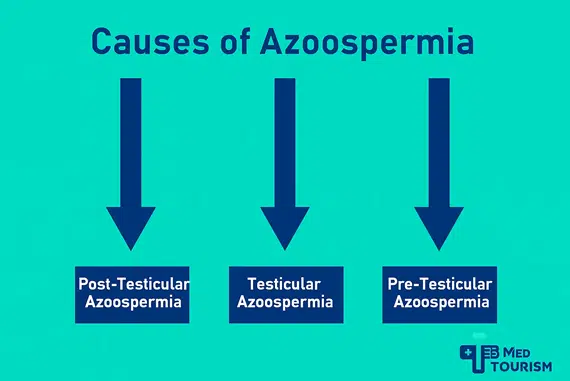
Different types of azoospermia
There are three types of azoospermia:
- Post-testicular azoospermia: A blockage or missing link along your reproductive path is known as post-testicular azoospermia. For whatever reason, your sperm production is being prevented from leaving. Another name for this kind is obstructive azoospermia. It is the most prevalent kind, affecting as many as 40% of azoospermia patients.
- Testicular azoospermia: A disease in (or damage to) the structure or function of your testicles causes testicular azoospermia, which is characterized by a weak or no sperm count. This condition is occasionally referred to as nonobstructive azoospermia.
- Pretesticular azoospermia: Your testicles and reproductive tract seem normal, but you don’t have enough hormone stimulation to produce sperm if you have pretesticular azoospermia. Hormone imbalance or chemotherapy may be the cause of this. Another name for this is nonobstructive azoospermia.
What are the symptoms of azoospermia?
Until you start unsuccessfully attempting to conceive with your spouse, you typically aren’t aware that you have the problem. Some people experience symptoms that are connected to the root cause. For instance, a hormonal imbalance or an infection-related tumor on your testicles may be the cause of your low libido.
Otherwise, possible symptoms might include:
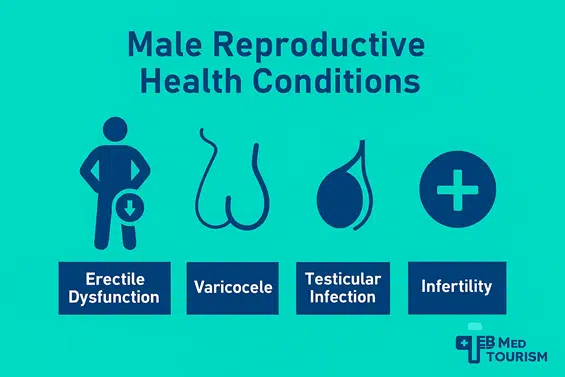
- Low sex drive
- Erectile dysfunction
- Lump, swelling, or discomfort around the testicles
- Decreased hair on the face or body
What are the causes of azoospermia?
One of the most common azoospermia causes is obstruction or blockage, although other causes include hormone imbalances or genetics.
Post-testicular azoospermia (obstructive azoospermia)
The ejaculatory duct (the tube that sperm pass through to mix with fluid and create semen), the vas deferens, and the epididymis (the corkscrew-shaped duct where sperm develop) are the areas where blockages most occur. These impediments effectively create a blockage that prevents sperm from exiting your testicles.
Problems that can cause blockages include the following:
- A testicular injury or trauma.
- Conditions (like epididymitis).
- Inflammation.
- Ejaculating backwards.
- Prior procedures on your pelvis.
- Growths or cysts.
- Vasectomy.
- Mutation in the gene for cystic fibrosis, which results in either a buildup of viscous secretions in the vas deferens (which prevents sperm) or the absence of vas deferens formation.
Pretesticular and testicular azoospermia (nonobstructive azoospermia)
Pretesticular and testicular azoospermia (nonobstructive) may stem from genetic disorders, endocrine imbalances, or undescended testicles, which are sometimes treated with orchiopexy.
Among the non-obstructive causes of azoospermia are hormone imbalances and heredity. As the term suggests, no impediment or obstacle is preventing sperm from forming.
Causes of pretesticular and testicular azoospermia include:
- Some genetic disorders, such as Y chromosomal deletion, Klinefelter’s syndrome, or Kallmann syndrome.
- Endocrine disorders and hormone imbalances, such as androgen, low testosterone, and hyperprolactinemia.
Varicocele. - Reactions to specific drugs that could impair the production of sperm.
chemotherapy, radiation therapy, or exposure to poisons or heavy metals. - Either without testicles or having testicles that are not descended.
- Orchitis.
- Lifestyle decisions such as abusing alcohol or drugs and spending a lot of time in bathtubs or saunas.
How is azoospermia diagnosed?
If, on two different occasions, your semen examination reveals no sperm, your doctor will diagnose you with azoospermia. In most cases, a sperm study is performed after a couple has failed at becoming pregnant.
Diagnosis without testing
Your doctor will review your complete medical history in order to determine the reason for azoospermia. This includes asking about:
- Your prior fertility.
Injuries or procedures involving the pelvis. - Infections such as sexually transmitted infections (STIs) or urinary tract infections (UTIs).
- Your past and present prescription drugs.
- Any usage of drugs, alcohol, or marijuana.
- Exposure to heat or sauna use.
- A family history of infertility, cystic fibrosis, or birth defects.
A comprehensive physical examination will also be performed by your healthcare practitioner, who will pay particular attention to the areas of your scrotum. A rectal examination could also be part of it.
Tests needed to diagnose azoospermia
Your healthcare provider may also order the following tests:
Follicle-stimulating hormone (FSH) and testosterone levels are measured by blood testing.
Genetic analysis.
Scrotal ultrasounds or X-rays.
MRI (magnetic resonance imaging) of the brain if they think your pituitary or hypothalamus is involved.
Ways to Treat Azoospermia
The cause of azoospermia determines how to treat it. Understanding and treating azoospermia frequently involves genetic testing and counseling. Among the methods of azoospermia treatment are:
- If your azoospermia is caused by a blockage in your tubes and ducts, you may need surgery to unblock them or to reconstruct and connect those that aren’t enabling sperm to pass through.
- If the primary cause is low hormone production, prescription hormone therapies may be necessary.
- Extracting sperm using a needle straight from your testicle. By obtaining sperm in this manner, you can use assisted reproductive technologies such as intracytoplasmic sperm injection (ICSI) or in vitro fertilization (IVF) to become pregnant.
Your doctor might provide genetic counseling if the cause of azoospermia is believed to be something that could be inherited by offspring.
Having a baby despite azoospermia
There are a number of assisted reproductive methods and therapy alternatives that may enable the birth of biological children, depending on the kind of azoospermia.
Direct sperm removal from the testicle may enable in vitro fertilization (IVF) in cases of obstructive azoospermia. In fewer instances, surgery to clear the obstruction may also be considered.
The likelihood that a biopsy would reveal viable sperm in the testicles is a critical factor in determining the course of action in cases of secretory azoospermia.
Couples may think about sperm donation in Iran if sperm retrieval is not an option, but they should examine ethical and religious perspectives and questions, such as, “Is sperm donation haram by Islamic law?” Additionally, several nations use sperm bank birth limits to control the maximum number of children that can be born from a single donor.
Testicular biopsy or TESA
Direct sperm extraction from the testicles can be accomplished by testicular biopsy or testicular sperm aspiration (TESA). In order to maintain the male’s genetic load and achieve conception, viable sperm can be used in an in vitro fertilization (IVF) procedure.
TESE
Both obstructive and non-obstructive azoospermia in males are treated with TESE. Due to either a partial or total failure in sperm production in the testes or an obstruction in the pathway between the ejaculatory system and the location of sperm production (the testes), these men do not have sperm in their ejaculate.
PESA (Percutaneous Epididymal Sperm Aspiration)
For men with obstructive azoospermia from a previous vasectomy or infection, PESA is a procedure used to retrieve sperm for IVF/ICSI. In conjunction with the retrieval of their female partner’s eggs, it is performed under local anesthetic in an operating room or office.
Micro-TESE
Under a microscope, Testicular Sperm Extraction (TESE) literally means removing the relevant seminiferous tubules from the testicle’s inner tissue in order to separate any living sperm that may be present.
Azoospermia treatment is carried out under the proper anesthesia following the sperm analysis, required hormonal and genetic testing, and physical evaluation of the applicants. General, regional, and local anesthesia are all possible.
The choice of anesthesia technique is made jointly by the patient and the doctor. A tiny incision is made in the sac known as the scrotum, which contains the testicle, to perform the surgery.
Sperm are then looked for under a microscope in appropriate tissues. The process can take up to two hours because it must be repeated until sperm is found.
IVF and ICSI
Two advanced reproductive treatments, Intracytoplasmic Sperm Injection (ICSI) and In Vitro Fertilization (IVF), are commonly used to help men with azoospermia become pregnant when sperm can be recovered from the testicles. Here are the differences and how each procedure differs:
- IVF: IVF allows fertilization to happen naturally outside the body by combining sperm and eggs in a lab dish. When there are enough viable sperm that can swim and fertilize an egg on their own, IVF is usually performed. It works better for situations of obstructive azoospermia, in which sperm are normal but prevented from ejaculating, or mild male infertility.
- ICSI: When there are few or low-quality sperm available due to severe male infertility, such as non-obstructive azoospermia, ICSI is a specialized type of IVF. Therefore, ICSI is the best option when the sperm must be surgically removed from testicular tissue (for example, using TESE or Micro-TESE), the sperm count is very low, or the sperm motility is low.
In summary, despite IVF that relies on sperm naturally penetrating the egg in a lab setting, ICSI bypasses that process by manually injecting a single sperm into an egg, making it a more precise and effective method for azoospermia treatment.
These methods give hope to couples seeking infertility treatment in Iran, where advanced fertility centers offer affordable and high-quality care.
Azoospermia Treatment Cost
In terms of azoospermia treatment cost, diagnostic tests such as semen analysis, hormonal testing, and testicular biopsy can range from $1,000 to $7,000.
In terms of azoospermia treatment cost, diagnostic testing alone—such as semen analysis, hormone and genetic testing, imaging, and possible testicular biopsy—can range from $1,000 to $7,000.
Whether the condition is obstructive (caused by a blockage) or non obstructive azoospermia (caused by hormonal, genetic, or testicular issues), the cost could be different.
Procedures like TESE in Iran or micro-TESE surgery for non-obstructive situations, as an azoospermia treatment cost, can cost $5,000 to $10,000+, while surgical procedures such as sperm retrieval or vasectomy reversal can cost $3,000 to $10,000.
The prices increase if assisted reproductive technology (ART) like IVF in Iran or ICSI in Iran is required. Typically, these procedures range from $15,000 to $20,000+, plus additional charges for sperm freezing and storage.
Consultations, medicine, and potentially several IVF cycles increase the overall cost of treating azoospermia to a range from $5,000 to more than $30,000.
Is it possible to prevent azoospermia?
No, it’s not. One of the azoospermia causes is inherited abnormalities that cannot be prevented. Here are several ways to reduce the likelihood of azoospermia if it is not a genetic condition:
- Stay away from activities that could harm your reproductive organs, or wear protective gear (e.g., a baseball cap).
- Avoid radiation exposure whenever you can.
- Recognize the advantages and disadvantages of drugs that may impair sperm production.
- Limit the amount of time your testicles are exposed to high temperatures.
Conclusion
Azoospermia, or zero sperm count, is a severe but curable cause of male infertility. TESE, Micro-TESE, IVF, and ICSI are examples of reproductive medicine advancements that have enabled many men with obstructive and non-obstructive azoospermia to become biological fathers.
Early diagnosis, a suitable medical evaluation, and expert fertility management are essential for success. TebMedTourism offers couples seeking affordable, high-quality fertility choices excellent access to Iran’s leading infertility specialists and state-of-the-art treatment centers. In order to ensure a safe, simple, and economical transition to motherhood,
TebMedTourism provides a comprehensive variety of medical tourism services, from free consultation and visa assistance to hospital arrangements and lodging.
Can you still get pregnant with azoospermia?
Yes. Even if there are no sperm in the semen following IVF or ICSI treatments, pregnancy is still possible when healthy sperm are collected directly from the testicles using techniques like TESE or Micro-TESE.
Will sperm come back after azoospermia?
In some cases, yes. If azoospermia is caused by a hormonal imbalance or blockage, treatments such as hormone therapy or surgery may restore sperm production or flow. However, in genetic or severe testicular cases, sperm may not return naturally.
How rare is azoospermia?
Azoospermia affects about 1% of all men and 10% of infertile men. It’s uncommon but still one of the major causes of male infertility
How long does it take to treat azoospermia?
Treatment duration varies depending on the cause. Hormone therapy may take a few months to restore sperm production, while surgical procedures like TESE or micro-TESE take only a few hours, followed by recovery and fertility treatment (such as IVF/ICSI), which can take several weeks per cycle.
How much does azoospermia treatment cost?
Diagnostic tests cost $1,000–$7,000. Surgical treatments like TESE or micro-TESE cost $5,000–$10,000+. IVF or ICSI range from $15,000 to $15,000–$20,000+. Overall, depending on complexity and the number of IVF cyclestreatment can cost $5,000–$30,000+.