
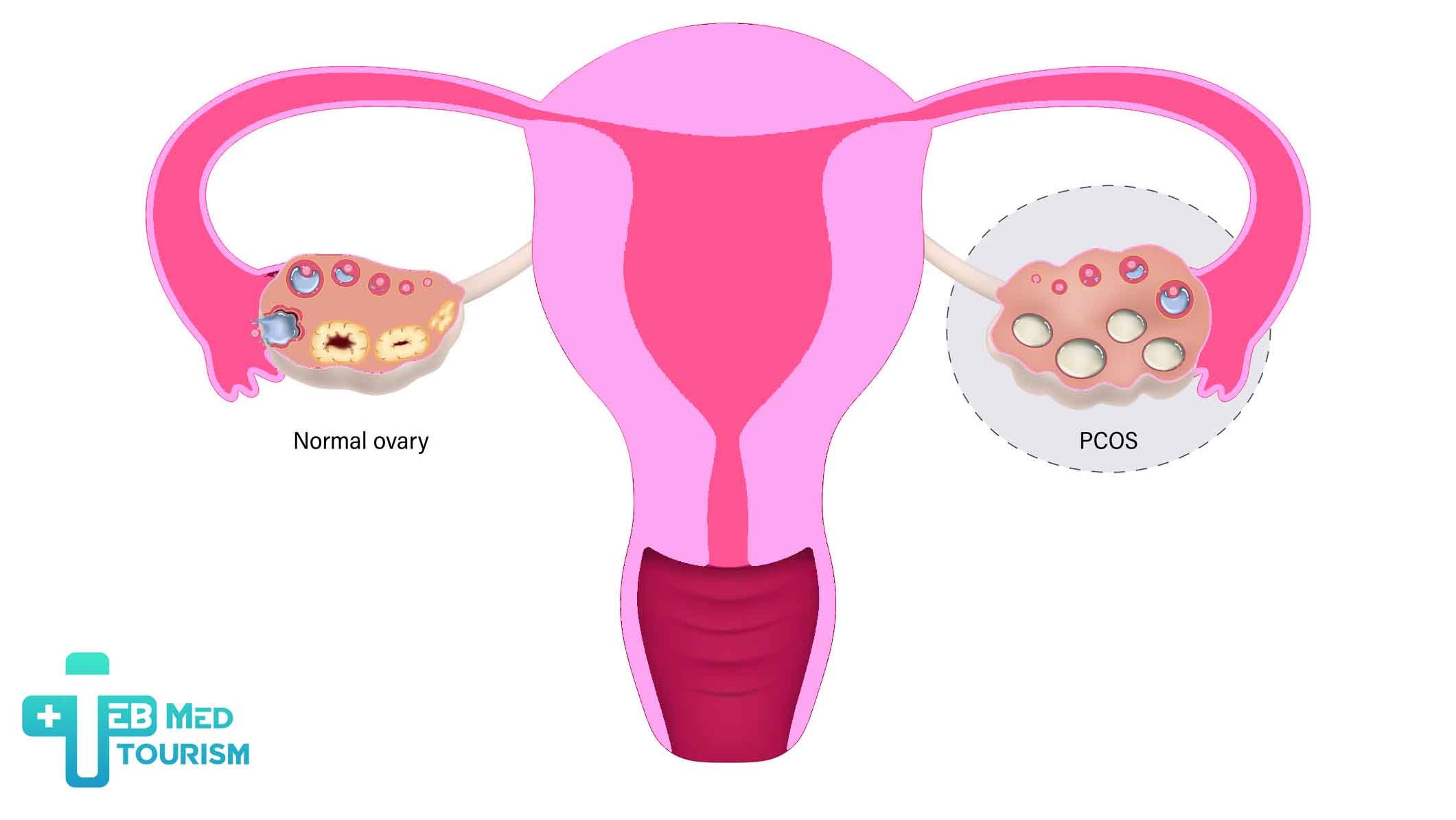
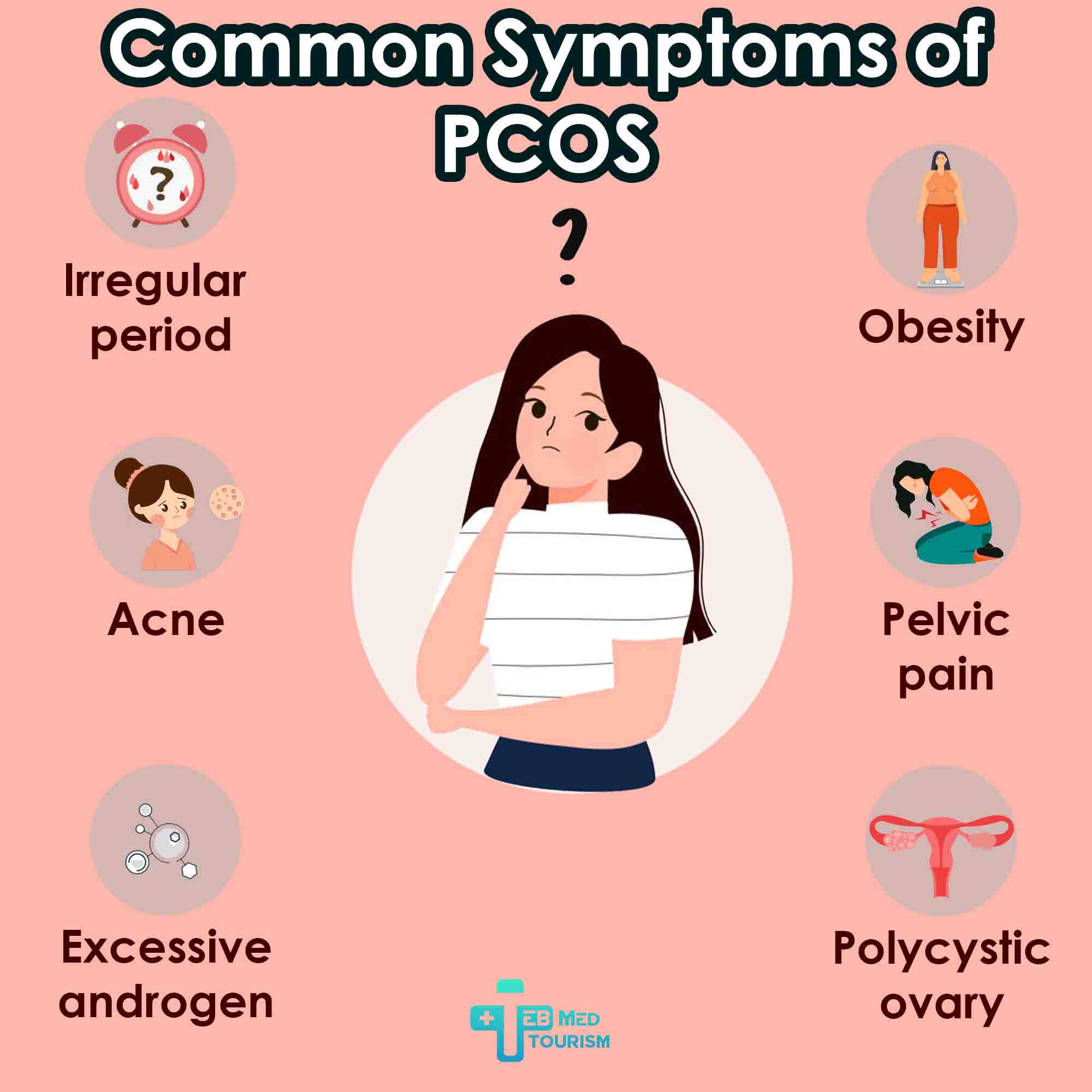
PCOS manifests through diverse symptoms that vary in intensity among individuals. Recognizing PCOS symptoms is crucial for early diagnosis and management, which can enhance quality of life. A diagnosis typically requires at least two of: irregular periods, elevated androgen levels, or polycystic ovaries on ultrasound. Below is an overview of the primary PCOS symptoms and their impacts.
Individuals with these signs should consult a healthcare provider. Early intervention can alleviate PCOS symptoms and reduce risks like diabetes.

Can PCOS Cause Infertility? Having Polycystic Ovary Syndrome (PCOS) does not equate to being unable to conceive. PCOS is a frequent yet manageable factor contributing to fertility issues in women. The hormonal imbalance associated with PCOS can disrupt the development and release of eggs during ovulation. Lack of ovulation translates to inability to conceive. For understanding more about PCOS and infertility, you can follow our topic by clicking here. In TebMedTourism, our consultant here to answer your question about PCOS and infertility, and also any other infertility related topics

Comments & Questions