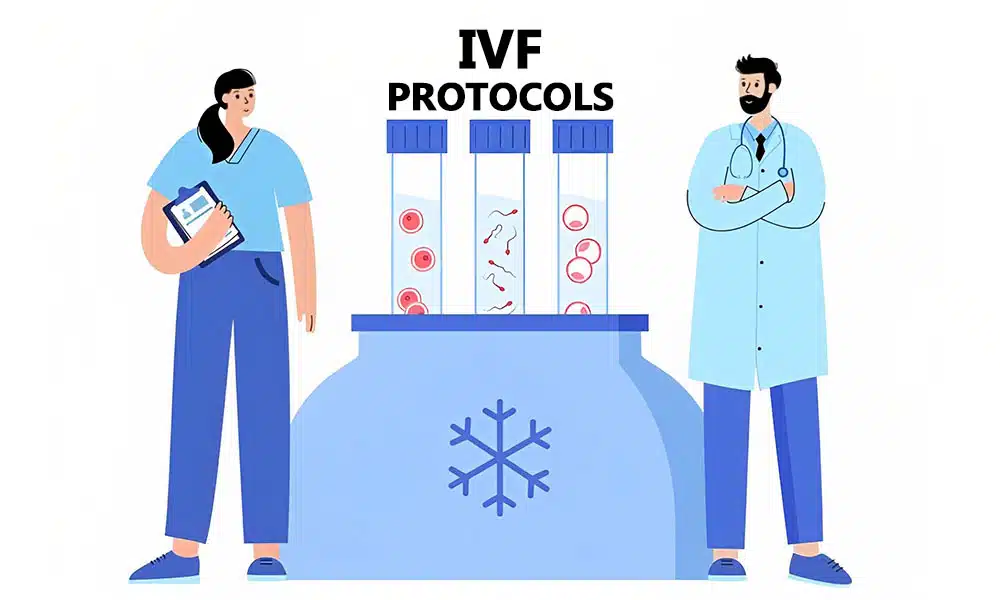
In order to undergo the IVF process, there are several IVF protocols that can be used to stimulate the ovaries by the use of certain medications and prepare them for in vitro fertilization (IVF). This process is done in order to reach an optimal number of eggs to be fertilized and make healthy embryos so that at least one pregnancy occurs.
There are different types of IVF protocols and each of them can be suitable for certain patients. For choosing the best IVF protocol, you need to consult with your fertility doctor to review your medical records (woman’s age, response to the medication and the outcome of previous attempts) and decide which protocol is right for you.
IVF Protocols
Antagonist Protocol (Short Protocol)
This is the most commonly used protocols for IVF. It is effective for most of the patients and contains the lowest number of injections. In this protocol, you will be informed to use birth control pills before starting the IVF cycle. For 10 days you will be taking follicle-stimulating hormone (FSH) and will have luteinizing hormone (LH) injections.
Around the day 5, the Gonadotropin-Releasing Hormone (GNRH) antagonist is used in order to prevent premature ovulation. Your doctor may use “Lupron trigger” or “dual trigger” medicines to stimulate the maturation of the eggs before retrieval process begins. In this way the risk of Ovarian Hyper-Stimulation Syndrome (OHSS) decreases significantly.
Lupron Down Regulation (Long Lupron Protocol)
This protocol is mostly used in the younger patients or those who had poor-quality embryos in their previous protocols. You will be prescribed to take birth control pills before starting the cycle of IVF. On the third week your doctor will order an injectable medication called Lupron. By undertaking Lupron injections, your pituitary gland temporarily stops secretion of FSH and LH hormones. Injections can control the cycle and prevent premature ovulation of the follicles.
The Micro-dose Lupron Flare Protocol
The micro-dose Lupron is prescribed for those patients who had a poor response to their previous protocols due to their high reproductive age or low ovarian reserve. The flare protocol is used to make the ovaries quickly respond to the stimulation and produce enough mature eggs to be used in the IVF process. The lower dose of Lupron stimulates the body’s natural FSH production instead of suppressing it. Taking micro-dose Lupron for stimulation phase continues until the injection of the Human Chorionic Gonadotropin (HCG) trigger. This protocol usually makes the IVF process work by enhancing the response speed of the ovaries.
Estrogen Priming Protocol
Women who respond poorly to the short protocols and have low ovarian reserve may enhance their ovaries response by using this protocol. Estrogen Priming Protocol synchronize more follicles for retrieval. For this aim, your fertility doctor may suggest you to undergo an estrogen medication and probably a few days of GNRH antagonist before you start the IVF cycle.
Mini-IVF or Micro-IVF Protocol:
Some experts believe that minimal stimulation may offer some benefits instead of using traditional treatment. The related doctor may prescribe fertility pills or medications in very low dosage in order to retrieve just one or two eggs each time. The disadvantage of using this protocol is that it produces just a few healthy eggs and it needs undergoing more egg retrievals for achieving the goal of getting pregnant.
What is a typical IVF protocol?
Which is better; short or long IVF protocol?
Both short and long protocols of IVF are practical ways for stimulating egg follicles’ growth and retrieving them for insemination. Long IVF protocol which is known as GnRH agonist long protocol will take about 4-5 weeks. You will start taking medications on the 21st day of your menstruation cycle which is known as ‘down regulation’ and aims to suppress ovarian function. Typically, after 10-14 days of suppressing the ovaries, the second type of medication which is gonadotrophins (typically FSH or hMG) will be started and it will be administered for 12-14 days. Gonadotrophins stimulate follicles growth and you will be checked by ultrasound every 3-4 days during this process to monitor the response of follicles to the medications and determine the time of egg retrieval. A short protocol will take 2 to 3 weeks and usually consists of 10-12 days of medication before egg retrieval. In the short protocol, there is no suppression of ovarian functions. You should take Gonadotrophins (FSH or hMG) for about 10-12 days and while the follicles are growing, you need to be checked by your doctor through internal scans every 3-4 days. The long protocol was the first IVF protocol that was used for patients and after that short protocol was developed. Studies have shown that there is little difference in the results of long and short IVF protocols. However, a short IVF protocol is less prone to Ovarian Hyperstimulation Syndrome (OHSS). There is no fixed protocol for all patients and treatment plans should be arranged according to the individual’s medical history and follicles prognosis. TebMedTourism’s doctors will carefully consider the medical condition of each patient and then arrange the best IVF protocol.
What is the best IVF Protocol?
It is fair to say that the best IVF protocol is neither maximal nor minimal, instead of them, it should be optimal based on the patient’s age, medical history, basal follicle count, Anti-Mullerian Hormone (AMH) levels, and family building aims. Before starting the IVF cycle, you have to consult with your fertility doctor to find out which protocol best fit your condition. In TebMedTourism company, by introducing you to our professional team, we pave the way of your fertility treatment. For getting more information, contact us now and consult with our experts free of charge.
What is the best IVF protocol for a poor responder?
Does IVF protocol affect egg quality?
Does long protocol IVF produce more eggs?
Studies have shown that there is little difference in the result of IVF protocols but the short protocol has less risk for OHSS compared to long protocol. In the long IVF protocol, the doctor tries to stimulate the patient’s ovaries by using certain drugs one week before her menstruation cycle starts. These medications suppress two hormones called Follicle Stimulating Hormone (FSH) and luteinizing hormone (LH) which are made in the pituitary gland and cause your ovary to make eggs. By suppressing these two hormones, the ovaries become suppressed and do not make eggs, and the ovarian hormone is called estradiol. Once the ovarian function has been suppressed, usually after 10-14 days, you will start taking the second set of medication which is named gonadotrophins, and should be administered for 12-14 days. Gonadotrophins stimulate follicles’ growth and prepare them for egg retrieval. During this time, you will be monitored every 3-4 days to evaluate the medication effects on your follicles.