IVF failure is a frustration experienced by some IVF patients on their first attempt for a variety of reasons. IVF in is one of the most effective treatments for infertility. None of the clinics will guarantee a 100% IVF success rate for the procedure, even if you seek the best IVF clinic in your area.
Sometimes the IVF failure rate can be discouraging, especially for couples who enter the process with high hopes. When IVF fails in early stages, it may feel devastating, yet understanding the common causes and solutions can help guide your next steps.
This article will help you identify the most common reasons for IVF failure and what you can do if IVF keeps failing.
What are the Reasons for IVF failure?
IVF failures are mostly caused by hormonal imbalances, low-quality eggs or sperm, uterine issues (thin lining, inflammation), lifestyle factors (smoking, obesity), issues with the embryo (chromosome abnormalities, poor quality), etc.
We will consider some of the common reasons for IVF failure in the following:
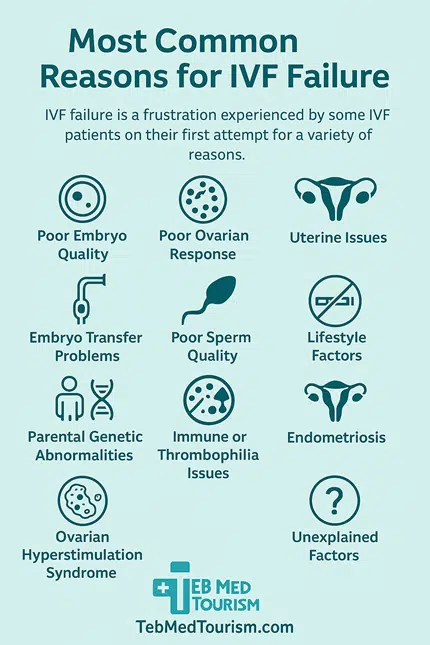
Poor Embryo Quality
The poor quality of the embryo is one of the main reasons that IVF in Iran or anywhere else fails. Many embryos have defects that prevent them from implanting once they are transferred to the uterus.
Defects can lead embryos to die rather than grow, even if they appear healthy in the lab. In almost all situations, the reason you are unable to conceive is not a problem with your uterus. Because it is not healthy enough to grow, the embryo does not implant.
Would you like to learn about “hatching in IVF”?
Poor Ovarian Response
Occasionally, a woman’s ovaries may not react to fertility medications sufficiently. When this occurs, the likelihood of IVF success rate decreasing is higher. A woman may not generate enough eggs to produce a number of embryos for screening and possible implantation, particularly if she is older than 37 or has higher FSH levels.
When this occurs, the likelihood of IVF failing increases. After reviewing the situation, your reproductive endocrinologist could adjust your fertility drugs for the subsequent IVF cycle.
After reviewing the situation, your reproductive endocrinologist could adjust fertility drugs for the subsequent cycle in order to improve outcomes.
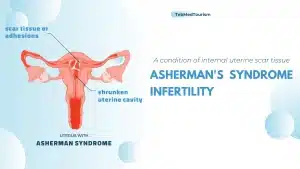
Uterine Issues
The most crucial organ for ensuring the fetus develops normally during the whole pregnancy is the uterus. The healthy growth of the fetus may be affected in women with uterine anomalies such as adhesions, fibroids, or poor lining. This can disrupt the IVF cycle timeline and may also be the primary cause of failed IVF rounds.
Embryo Transfer Problems
One major reason IVF keeps failing is difficulties during the transfer itself. Optimizing embryo transfers by using advanced techniques and timing analysis such as ERA can significantly improve results.
Chromosome defects can cause even healthy-looking embryos to fail in the lab, and immune system dysfunction, infections, or inadequate blood flow can all lead to an unfavorable uterine environment.
Poor Sperm Quality
A healthy embryo can result from improved fertilization, which is facilitated by a healthy sperm. However, sperm quality and quantity may be poorer in guys with azoospermia, which can have a direct impact on the IVF treatment’s outcome.
The likelihood of creating an embryo with chromosome abnormalities is increased by poor sperm quality. These embryos not only increase chances of IVF success but also raise miscarriage risks.
Lifestyle Factors
Lifestyle plays a huge role. Women who want to begin IVF treatment must quit smoking and adopt an IVF diet rich in antioxidants, healthy fats, and vitamins for at least three months to improve outcomes. Compared to women who do not smoke, smokers require twice as many IVF rounds to conceive and have a significantly higher risk of miscarrying.
There is a lower chance of effective IVF treatment for women who are underweight or overweight. It all comes down to keeping a healthy weight. Even a small weight loss of 10 percent can have a significant impact on your chances of becoming pregnant if you are overweight.
Parental Genetic Abnormalities
One of the main causes of miscarriages is linked to genetic abnormalities. In addition to raising the possibility of IVF failure, patients with parental genetic diseases may give birth to a kid that has many problems.
Parental genetic issues can lead to repeated IVF effects like miscarriages or embryo abnormalities. Genetic testing is often recommended before another attempt.
Immune or Thrombophilia Issues
Immunological and thrombophilia issues that interfere with embryo implantation can lead to IVF failure. While thrombophilia, a bleeding disorder, can result in microthrombi that block blood supply to the uterus, certain immunological dysregulations may cause the body to unintentionally attack the embryo.
These conditions are associated with recurrent implantation failure, especially in certain circumstances like antiphospholipid syndrome, even if there is currently not enough evidence to recommend comprehensive screening for all thrombophilias and immunological variables in IVF patients.
Read more: IVF and autism
The abovementioned issues are common reasons couples extend their IVF journey with additional treatments such as blood thinners or immunotherapies. Blood thinners or immunosuppressants may be used in some circumstances under strict medical monitoring.
Endometriosis
One prevalent cause of infertility is endometriosis. This can occur when endometrial tissue implants around the fallopian tubes or ovaries, where it may also result in scarring and inflammation.
A lower IVF success rate is associated with advanced endometriosis. It frequently degrades the quality of eggs and may have an adverse effect on implantation.
A lower success rate with IVF and IVF failure is linked to advanced endometriosis. One important aspect in explaining this negative effect has been identified as surgical injury to the ovarian reserve after endometrioma removal.
Ovarian Hyperstimulation Syndrome
Ovarian Hyperstimulation Syndrome (OHSS), which is mainly treated with preventative measures rather than directly causing IVF failure, can make IVF less successful by producing ovarian enlargement, fluid accumulation, and hormonal imbalances that impair implantation.
The main result of severe OHSS is that the current IVF cycle is essentially delayed or stopped by delaying the embryo transfer until hormone levels stabilize. OHSS can delay transfers, forcing a break between IVF cycles until hormone levels stabilize.
Unexplained Factors
Sometimes the question of why IVF fails has no known cause. It can be quite regrettable that doctors frequently call it unexplained infertility. Despite extensive examination, the cause is still unknown. It can be annoying.
Trial and error is a part of treatment. Multiple methods are tested. The most important thing here is patience. It’s also critical to maintain optimism.
With every try, additional details are revealed. Over time, understanding changes. Unknown causes of unexplained IVF failure occur when a successful egg retrieval, fertilization, and transfer of an apparently high-quality embryo do not result in implantation.
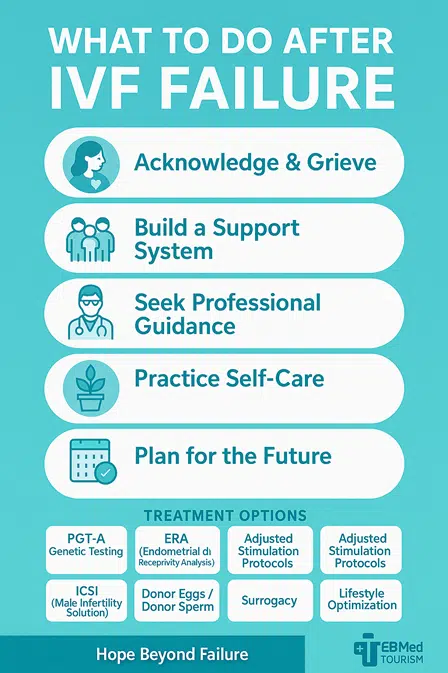
How To Cope With IVF Failure?
IVF failures affect not just your physical health but also your mental health. After an unsuccessful IVF attempt, you can be suffering through multiple phases of mourning until you find hope once more.
Acknowledge and Grieve
- Accepting sadness after the 1st IVF failure is natural. Give yourself time to experience depression after IVF, as well as grief and disappointment; these are natural emotions.
- Spend some time focusing on your mental health and grieving without passing judgment.
- Write in your journal, cry, or talk to a trusted person to express your feelings.
Build a Support System
- Surround yourself with supportive family, friends, or support groups who understand the pain of IVF fail. Use open communication and mutual support to rely on your relationship.
- Make contact with friends and relatives who can offer sympathy and understanding.
- To exchange stories with people who have gone through similar struggles, join a support group.
Seek Professional Guidance
- To manage anxiety and depression, speak with a mental health specialist who specializes in infertility.
- Review the unsuccessful cycle, look into the reasons, and talk about your options for the future with your infertility specialist.
Practice Self-Care
- Take part in relaxing activities and pursuits that make you feel happy and at ease.
- Maintain a healthy lifestyle by getting enough sleep, exercising, and eating a balanced diet.
- Treat yourself with kindness and stay away from needless triggers, like offensive material on social media.
Plan for the Future
- Take some time to feel better physically and emotionally before making any new decisions.
- Discuss potential reasons for the failure with your doctor and consider other options like PGT-A or modified protocols and choose the best IVF protocol.
- Rekindle your passions and remind yourself that your identity is not entirely defined by your role as a parent.
Is There Treatment for Recurrent IVF Failure?
Yes, recurrent IVF failure, also known as Recurrent Implantation Failure (RIF), can be treated by treating the underlying causes, some of which include immunological variables, blood coagulation disorders, and anatomic abnormalities. Let’s consider the above and some other treatments for recurrent IVF failure in the following:
Preimplantation Genetic Testing (PGT-A/PGS)
Before transferring embryos, the IVF add-on known as Preimplantation Genetic Testing for Aneuploidy (PGT-A), formerly known as PGS, checks them for aneuploidy, or an abnormal number of chromosomes.
To increase the likelihood of a successful pregnancy and lower the danger of miscarriage, a biopsy of a small number of the embryo’s cells is extracted, and the cells are then examined to identify euploid (normal) embryos for transfer.
Endometrial Receptivity Analysis (ERA)
In order to identify a woman’s unique “window of implantation” (WOI) for embryo transfer—the time when her endometrium is most receptive to an embryo—the Endometrial Receptivity Analysis (ERA), a customized embryo transfer test in IVF, examines a uterine lining biopsy.
Doctors can more accurately time the progesterone and embryo transfer by using the ERA test to classify the endometrium as receptive, pre-receptive, or post-receptive based on gene expression patterns. Patients who have experienced repeated implantation failure following prior IVF cycles with high-quality embryos are frequently given this option.
Hysteroscopy
Doctors can directly view and evaluate the inside of the uterus via a hysteroscopy, a minor surgical procedure performed prior to IVF, in order to detect and perhaps cure conditions including fibroids, polyps, and scar tissue that may impede embryo implantation and a successful pregnancy.
It helps to provide the best uterine environment for embryo transfer and is a useful diagnostic and therapeutic tool, especially for patients who have a history of unsuccessful IVF cycles. However, it is not always routine advice for every patient.
Adjusted Stimulation Protocols
In IVF treatment, adjusted stimulation protocols tailor ovarian stimulation by changing drug types (agonist, antagonist, or milder regimens), dosages, and timing to a patient’s ovarian reserve, past IVF results, age, and body mass index.
The goal is to maximize egg quantity and quality while reducing risks such as ovarian hyperstimulation syndrome (OHSS).
Typical modifications to enhance efficacy and patient experience include utilizing oral drugs like letrozole, modifying gonadotropin dosages, or moving from lengthy agonist protocols to shorter antagonist or minimum stimulation regimens.
Intracytoplasmic Sperm Injection (ICSI)
A specific type of IVF called intracytoplasmic sperm injection (ICSI) uses a micropipette to inject a single sperm directly into an egg rather than depending on the sperm fertilizing the egg on its own.
In order to enable couples to have a genetically related kid, this approach is mostly utilized to overcome male infertility, such as very low sperm count, poor sperm motility, or aberrant sperm shape.
Similar to a typical IVF cycle, the resultant embryo is grown in the laboratory after fertilization before being placed in the uterus.
Treatment for Endometriosis
Some experts believe that surgical removal of the endometriosis is necessary even if IVF is required. The apparent justification for this is that the cysts will disrupt the IVF treatment cycle and lower the likelihood of IVF pregnancies.
Despite its apparent logic, this is incredibly illogical. Since endometriosis is external to the uterus and will not impact the embryos that implant there, there is no need to treat endometriosis directly if you have it and require IVF.
As a matter of fact, your chances of having a successful IVF procedure can be decreased by needless laparoscopic surgery. The ovarian reserve is further decreased when the chocolate cyst is removed because it damages the healthy ovarian tissue nearby.
Endometriosis patients already have a diminished ovarian reserve, and surgery just makes it worse. As a result, they are unable to produce high-quality eggs after undergoing IVF procedures.
Immunological Treatments
Intravenous immunoglobulin (IVIG), steroids, and intralipid infusions are examples of immunological treatments for IVF that are intended to modify the immune system’s reaction during IVF, especially for patients who have recurrent pregnancy loss (RPL) or repeated implantation failure (RIF).
As advised by the Human Fertilization and Embryology Authority (HFEA), these treatments should only be considered in certain circumstances and under close medical supervision because their efficacy is debatable, and some evidence points to serious potential harm without demonstrated benefit.
Donor Eggs or Sperm
IVF uses donor eggs or sperm when an individual or couple is unable to use their own genetic material because of infertility, genetic concerns, or personal preference. For elderly patients or those with poor egg quality, donor eggs from a young, viable donor greatly increase the likelihood of high-quality embryos and overall success rates.
When a male partner is unable to produce viable sperm, donor sperm is utilized by single women or same-sex couples in need of a sperm supplier. Double donation is the practice of creating embryos for transfer using both donor sperm and donor eggs.
Surrogacy
The majority of gestational surrogate pregnancies are obtained using in vitro fertilization (IVF). IVF is the process of creating an embryo in a lab using either an egg and sperm donor or the intending parents’ egg and sperm. After that, the embryo is placed inside the carrier’s uterus.
Lifestyle Optimization
Lifestyle optimization for IVF includes a balanced, whole-foods diet rich in antioxidants, vitamins, and healthy fats; maintaining a healthy weight; regular, moderate exercise; adequate sleep and stress reduction techniques; and avoiding harmful substances like tobacco, excessive alcohol, and caffeine.
These adjustments create a supportive environment, improve egg and sperm quality, regulate hormones, and enhance overall well-being, thereby maximizing IVF treatment success.
Supplements and Adjunct Therapies
Despite their growing popularity, there is conflicting information about the efficacy of supplements and supplementary therapy for in vitro fertilization (IVF). Particularly in specific patient categories, several supplements, including as CoQ10, melatonin, and DHEA, have the potential to enhance ovarian response and egg quality.
While vitamin D and omega-3 fatty acids may improve certain IVF results, myo-inositol may help women with PCOS. Treatments like testosterone and growth hormone are frequently used hastily without sufficient proof, and other treatments like heparin and low-dose aspirin have variable effects. Adopting a Mediterranean diet is a straightforward and advantageous dietary strategy.
Personalized IVF Protocols
To increase success rates and reduce dangers, customized IVF methods adjust the procedure to each patient’s particular traits, including age, ovarian reserve, and hormone levels.
Preimplantation genetic testing (PGT) and specialized embryo transfer procedures can be included in these personalized regimens, which can modify the kinds and dosages of fertility medications and track ovarian response with regular blood tests and ultrasounds. Each patient’s fertility journey should be more effective, less stressful, and more successful.
Positive aspects of IVF Failure
Even though a failed IVF cycle is a terrible experience, there are some possible benefits, such as learning more about the reasons behind infertility, having the chance to adopt healthier lifestyle choices, having the chance to explore other family-building options like adoption or using donor gametes, and having the chance to learn new coping skills with supportive counseling.
A failed cycle may also serve as a springboard for some people to consider other family structures or to concentrate on objectives other than starting a family.
How Long After Failed Implantation Will a Period Start?
Your period will typically start within a week to two weeks after a failed implantation, or by the time your progesterone support medication is discontinued. Your period may come on schedule or a little later if you are using IVF.
The precise date can be affected by variables like the individual’s hormone levels and the type of IVF treatment. If your period doesn’t arrive as expected or you have concerns, contacting your fertility specialist for personalized advice is recommended.
Conclusion
The IVF failure is emotionally draining regardless of whether this is the 1st IVF failure or whether it keeps failing in subsequent cycles. Couples may be frightened by the IVF failure rate, yet each failed effort also provides insight into possible symptoms and remedies for IVF failure.
IVF effects can be physically, emotionally, and financially demanding. Yet, with persistence, modern science, and medical support, each attempt brings patients closer to success.
It’s common to experience disappointment or even depression following an unsuccessful IVF attempt, but there are still choices accessible with the correct medical and mental support.
At TebMedTourism, we believe every failed attempt is not the end of the journey but a step toward new hope. If you reach out to our expert team, they will provide you with international patient support and affordable treatment plans to help you explore all possibilities—from IVF and genetic testing to surrogacy—while receiving continuous guidance at every stage.
What happens to your body after failed IVF?
Hormonal medications stop after IVF fails, resulting in a withdrawal bleed (your period) within 1-2 weeks. Following a failed IVF attempt, you can also experience physical exhaustion, bloating, or psychological distress like feeling helpless.
Why does IVF fail with good embryos?
Even high-quality embryos may not implant due to hidden genetic issues, uterine problems, immune responses, or timing mismatches. This is one reason the IVF failure rate exists despite good embryos.
Why does IVF fail the first time?
Poor embryo quality, problems with the uterine lining, or lifestyle choices are frequently the causes of the first IVF failure. A lot of couples have to make multiple attempts before they are successful.
What to do after failed IVF?
If IVF keeps failing, talk to your doctor about the cycle, think about PGT-A or ERA testing, improve your lifestyle with an IVF diet, and take some time to heal emotionally.
When should you expect your period after failed IVF?
Most patients get their period within 1–2 weeks after implantation failure or when progesterone support stops. Delays can occur depending on hormones, but if your period doesn’t arrive, contact your fertility specialist.