Infertility can be an emotional and challenging journey for many couples. However, modern advancements in reproductive medicine, such as Intracytoplasmic Sperm Injection (ICSI), offer a promising solution. Designed to address even the most complex cases of infertility, ICSI has brought the dream of parenthood within reach for countless individuals. Whether the issue lies in low sperm count, immotile sperm, or other male infertility factors, this groundbreaking technique provides new hope for building a family.
What is intracytoplasmic sperm injection, aka ICSI-ET cycle?
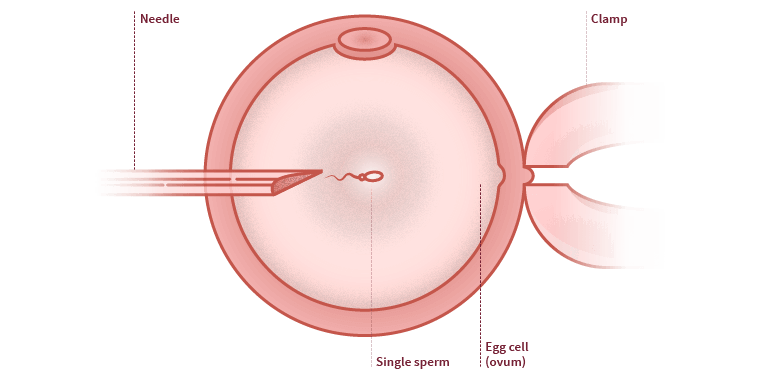
As the name suggests, intracytoplasmic sperm injection (ICSI) is a delicate procedure that involves injecting a single sperm into the cytoplasm of the woman’s egg, facilitating fertilization. Several eggs are treated with sperm and allowed to develop in culture fluid under carefully controlled conditions. The embryos that develop after 2–3 days, or blastocysts that develop within 5–6 days, are then transferred to the woman’s uterus, as in a standard IVF cycle. ICSI can be particularly helpful in cases of male infertility due to severe sperm abnormalities or when the male partner is disabled. It can also benefit couples facing infertility because the man has undergone a vasectomy that cannot be reversed. ICSI-ET cycle (complete cycle)

Who might need intracytoplasmic sperm injection?
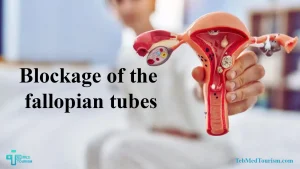
- Low numbers of sperm produced or ejaculated: This can result from retrograde ejaculation or a blockage in the vas deferens, the tubes that carry sperm out of the testes. A complete absence of sperm in the ejaculate can be addressed if sperm production occurs inside the testes. Surgical sperm retrieval methods are used to extract sperm, enabling intracytoplasmic sperm injection.
- Abnormal sperm that cannot swim well: Even when a sufficient number of sperm is present in the ejaculate, intracytoplasmic sperm injection can overcome the challenge of immobile sperm reaching the woman’s eggs.
- A previous vasectomy that cannot be successfully reversed.
- Problems with antibodies against sperm: These antibodies may be produced by the male partner in the ejaculate fluid or by the female partner in cervical secretions.
- Testicular cancer: This condition can occur in younger men, and treatment may impair sperm production. Sperm can be frozen before undergoing cancer treatment (which often has a high success rate), and the thawed sperm can later be used for intracytoplasmic sperm injection.
How is sperm collected?
The most common method is to use fresh ejaculate; however, this is not always possible for all male partners contributing sperm for intracytoplasmic sperm injection (ICSI). In some cases, surgical removal of sperm from the testes may be required. It is also possible to collect sperm from the urine if the man experiences retrograde ejaculation, where sperm travel backward into the bladder instead of forward into the penis. Men who cannot ejaculate due to nerve injury may be able to produce sperm through electro-ejaculation.

IVF with Intracytoplasmic Sperm Injection (ICSI)
Couples undergoing the ICSI-ET cycle, or intracytoplasmic sperm injection, experience a procedure very similar to in vitro fertilization (IVF). The woman first receives a course of hormone treatment to stimulate her ovaries to produce multiple eggs. These eggs are monitored via ultrasound, and once mature follicles have formed, the eggs are collected using a thin tube inserted through the vagina. The collected eggs are placed in a special culture fluid in the laboratory.
On the same day, sperm is collected, typically just before the egg retrieval. A single sperm is then injected into each egg. This process is repeated for all available eggs, which are cultured to determine whether they develop into embryos. The best-quality embryo at the 2–3-day stage or the strongest blastocyst at the 5–6-day stage is then transferred to the woman’s uterus. Different countries have specific regulations regarding the number of embryos that can be transferred. For example, in the UK, the limit is typically 1–2 embryos, while other countries may allow more, increasing the risk of multiple pregnancies.
How successful is intracytoplasmic sperm injection?
The success rates for ICSI are similar to those of IVF and depend on factors such as age and the stage at which embryos are transferred. Blastocyst transfer at the 5–6-day stage generally has higher success rates than embryo transfer at the 2–3-day stage.
Potential problems with intracytoplasmic sperm injection
Most children born as a result of ICSI are healthy. However, there is a risk that if the father produces abnormal sperm, the issue may be genetic and could be passed on to the child. Known genetic diseases may be tested using pre-implantation genetic screening (PGS), but no test exists for unidentified abnormalities.
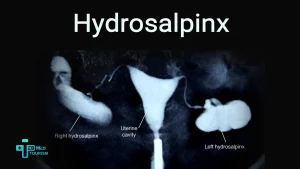
ICSI also carries the same risks as standard IVF, including an increased likelihood of multiple pregnancies, a higher risk of ovarian hyperstimulation in the female partner, and a greater chance of ectopic pregnancy due to implantation in the fallopian tubes.
The development of ICSI in Iran has been significantly influenced by collaborations between its pioneers and interdisciplinary experts, supported by the endorsement of Shia jurists.
Embryo Transfer (ET)
Embryo transfer is a straightforward procedure following ICSI and IVF, often considered the simplest and final step in the in vitro fertilization process. The goal of embryo transfer is to facilitate conception after successful fertilization.
When does the embryo transfer procedure occur?
Embryos are generally transferred to the woman’s uterus during the 2–8 cell stage. This typically occurs between days 2–4 after egg retrieval but may vary from day 1 to day 6. Some clinics allow embryos to develop to the blastocyst stage, which occurs around day 5, before transfer.
IVM-ET Cycle (Complete Cycle)
This cycle includes both in vitro maturation (IVM) and embryo transfer (ET), ensuring the best chances for conception through advanced reproductive techniques.