Orchiopexy, also known as orchidopexy medical term is derived from Greek, where “orchio” means testicle and “pexy” means fixation or suspension. So, you can guess the purpose of orchiopexy! It is a surgical procedure to:
- Move undescended (cryptorchid) testicles
- Resolve testicular torsion
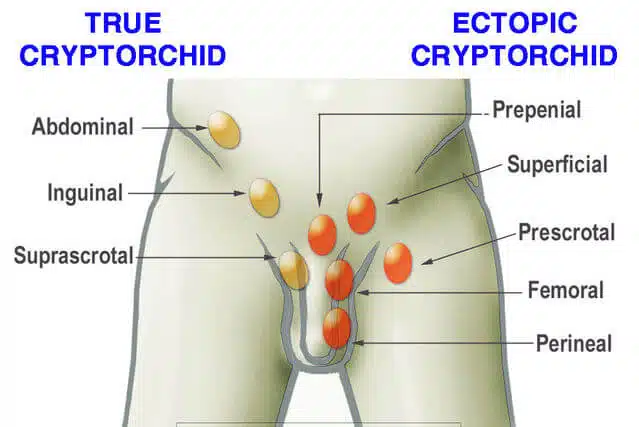
Cryptorchidism or undescended testicles is a common birth defect in males, where one or both testicles do not descend before birth. It affects around 2-8% of full-term male infants and about 33% of premature infants. Normally, the testes form in the abdomen and should descend into the scrotal area between twenty-five to thirty-five weeks of gestation. If the testicles do not descend before birth, doctors perform surgery called orchiopexy to relocate them to the scrotum. Researchers suggest that most cases of cryptorchidism do not resolve naturally, making orchiopexy surgery necessary. By performing orchiopexy before puberty, the risk of testicular cancer and infertility associated with cryptorchidism can be reduced, which we will discuss in detail in this article.
Why someone need orchiopexy surgery?
Orchiopexy is required in two situations:
- undescended testicle
- Retractile testicle
- Testicular torsion.
Normally, undescended testicles are altered in childhood to avoid future difficulties such as:
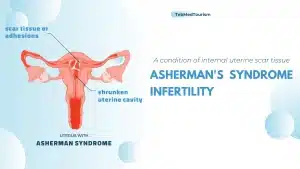
- infertility
- The enlarged threat of testicular tumors.
Undescended testicle
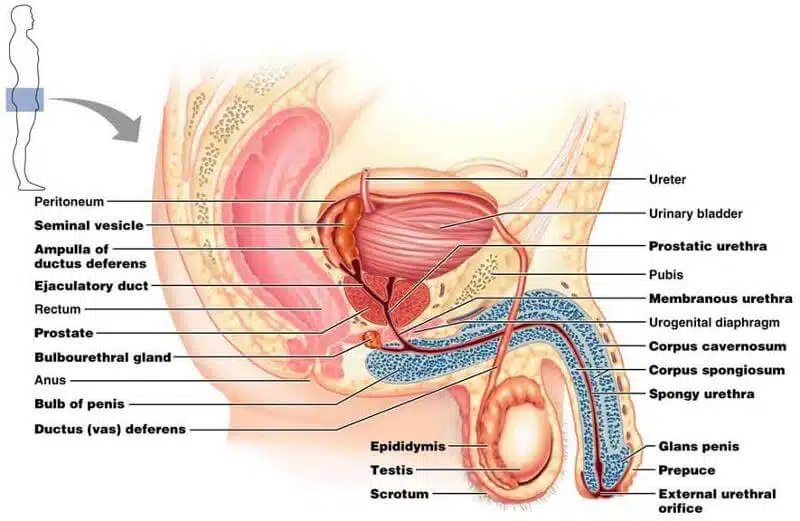
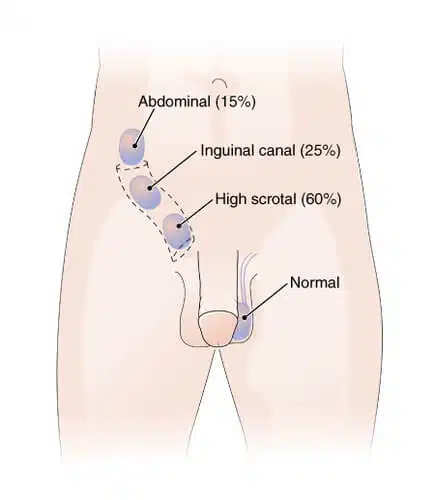
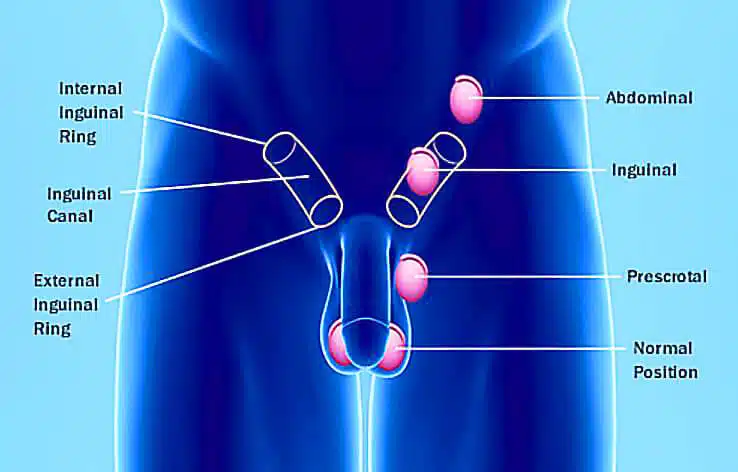
An undescended testicle, also known as cryptorchidism, is a condition in which one or both testicles cannot descend into the scrotum properly during fetal development. The testicles usually develop in the abdomen and into the scrotum before birth or during the first months of life. If they remain in the abdomen or anywhere along the way to the scrotum, it can lead to various symptoms and potential complications. Most of the time, it’s just a testicle that doesn’t descend into the scrotum, which is a pouch of skin that hangs below the penis.
But sometimes both testicles are affected and needed to cryptorchidism orchiopexy. According to National Health Service (NHS) of England, testicle will usually descend into the scrotum spontaneously by the time your baby is 3 to 6 months old. If the testicle does not descend after 6 months, it is very difficult to descend without treatment. In this case, a surgical procedure called Orchiopexy would be recommended to reposition one or both testicles. Orchiopexy should be done before your baby is 12 months old.
The ideal age for orchiopexy is between 6 to 12 months of your baby. Indeed, waiting longer than this time can increase a boy’s risk of developing fertility problems (infertility) or testicular cancer later in life.
Symptoms of undescended testicle
Early diagnosis and treatment of undescended testicles is important to avoid potential complications and improve fertility. If you think you or someone you know may have an undescended testicle, it is important that you see a health care professional who can perform a physical exam and recommend appropriate treatment options. Surgery is often needed to correct the condition and bring the testicle(s) into the scrotum. Here, we describe most common complication of undescended testis:
- Absence of testicles in the scrotum: The most obvious symptom is the absence of one or both testicles in the scrotum. It may be easier to just feel or see one testicle in the scrotum while the other is missing. The scrotum may be smaller or emptier on the side where the testicle has not descended.
- Palpable testicle in the inguinal canal: In some cases, the undescended testicle can be palpated in the groin or inguinal canal. The inguinal canal is the passage through which the testicles descend through the abdominal wall and into the scrotum.
Retractile testicle
Retractile testicles are occasionally confused with undescended testicles, but they should not be considered the same. Undescended testicles are not detectable in the scrotum, whereas retractable testicles reside there but can be retracted through muscle contractions. It’s important to note that, retractile testicles don’t require orchiopexy or other surgical procedure and treatment.
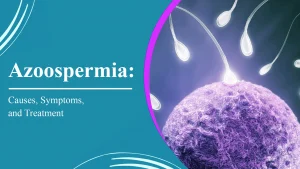
Testicular torsion
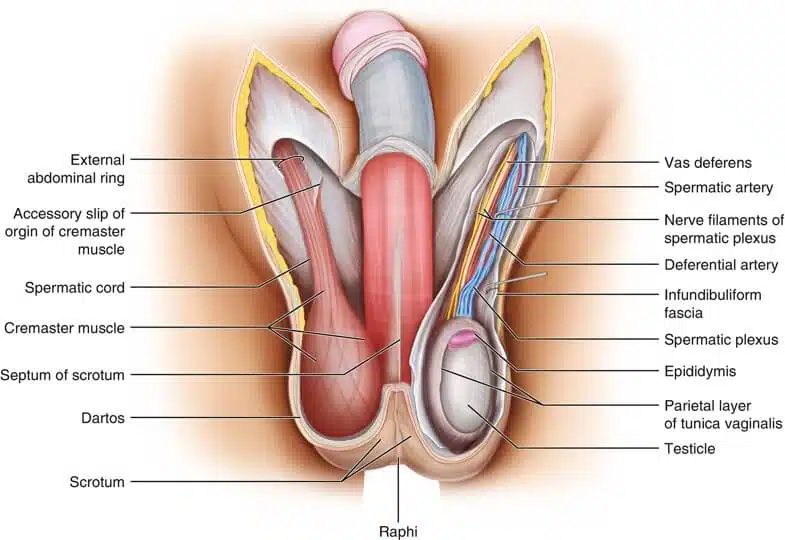
Testicular torsion is a condition where the spermatic cord that supplies blood to the testicle becomes twisted, which may result in reduced blood flow and damage to the tissue. Orchiopexy for testicular torsion involves securing the affected testicle in place to prevent future twisting and maintain blood supply. In cases of testicular torsion, the primary objective is to untwist the spermatic cord and restore blood flow to the testicle as soon as possible. This is typically achieved through emergency surgery known as detorsion or testicular fixation, which aims to prevent the recurrence of twisting. During orchiopexy for testicular torsion, the surgeon may take the opportunity to also secure the testicle in the scrotum to decrease the risk of future twisting. This can involve suturing the testicle to the scrotal wall or utilizing other techniques. This additional orchiopexy procedure is intended to stabilize the testicle and help prevent further twisting. It is crucial to recognize that testicular torsion is a medical emergency, and timely surgical intervention is essential to safeguard testicular function. If you suspect testicular torsion, seek immediate medical attention to prevent potential long-term harm to the testicle. The specific surgical approach and techniques used in orchiopexy for testicular torsion will depend on the severity of the condition and the surgeon’s discretion.
Diagnosis Orchiopexy
The diagnosis of cryptorchidism or UDT is exactly obvious by a lost testicle in the scrotum. The question is whether the testicle remains in the abdomen or the groin. The situation will be tough to recognize. Giving to one academic study, imaging like X-rays or CT scans is not going to be a valuable diagnostic instrument. If the undescended testicle cannot be felt, the next way to identify must be done by a specialist, such as an urologist.
This situation happens if the testicle has not inclined afterward the child is six months of age. Best diagnostic test in this situation will be ultrasonography. Parent whose kid has had the process is recommended to stay calm and keep their child calm and relaxed situation, before and after the procedure.
Delaying Treatment
This surgery is a voluntary operation nevertheless there is a danger of serious outcomes, if delaying treatment lasts too long. These complications include:
- Decreased fertility
- Testicular atrophy
- Testicular torsion
- Inguinal hernia
- Injury to the area that testicle is located
- Testicular tumor
The study has established that ones who had the process done before age 10 years old, their risk of testicular cancer decreased highly.
Orchiopexy surgery
Orchiopexy is a surgical procedure performed to correct undescended testicles (cryptorchidism) by moving it from its abnormal position in the abdomen or along the inguinal canal into the scrotum. Surgery is usually recommended for boys with undescended testicles and is usually done before the child is 12 months old. However, in some cases, it can be done later in childhood or adolescence. The success rate of orchiopexy nearly 100%. It may be unilateral or bilateral. If both testicles descend, it is called bilateral orchiopexy. Normally, this operation takes up to 90 minutes from anesthesia to recovery after surgery.
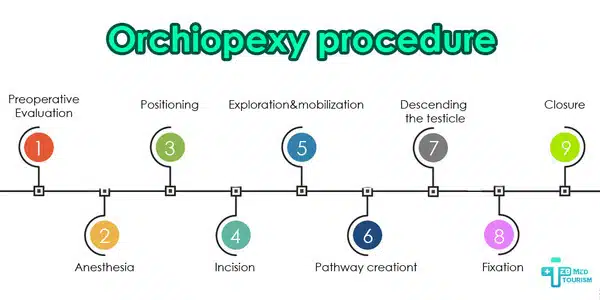
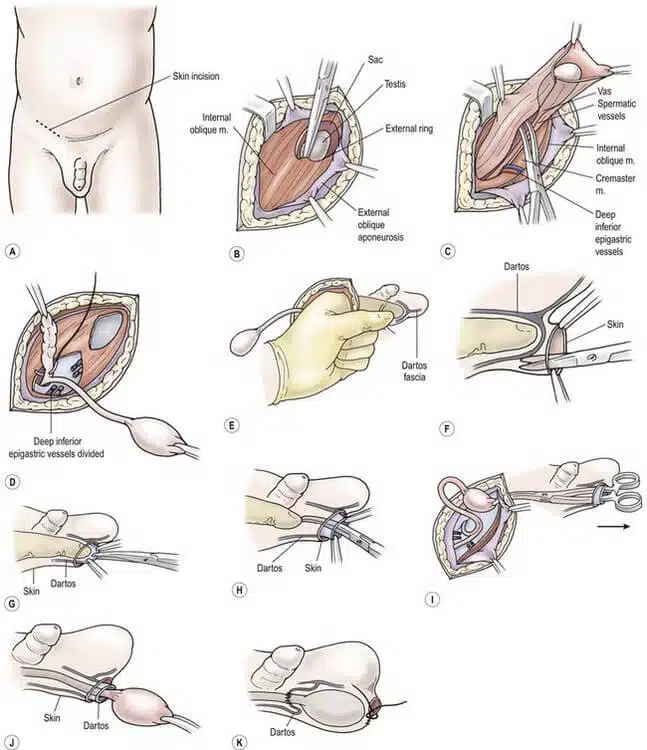
Orchiopexy surgical procedure
- Before surgery: your child will have a thorough evaluation, which may include a physical exam, imaging tests (such as an ultrasound), and hormonal studies. This evaluation helps determine the exact location of the undescended testicle and ensures that it is indeed not descending into the scrotum and cannot be retracted (a condition in which the testicle can be manually returned to the scrotum).
- Anesthesia: On the day of surgery, the child will be taken into the operating room and will be given general anesthesia. General anesthesia ensures that the child is asleep and pain-free during the procedure.
- Positioning: When the child is anesthetized, he or she will be positioned appropriately for surgery. The surgical team will ensure the comfort and safety of the child during the surgery.
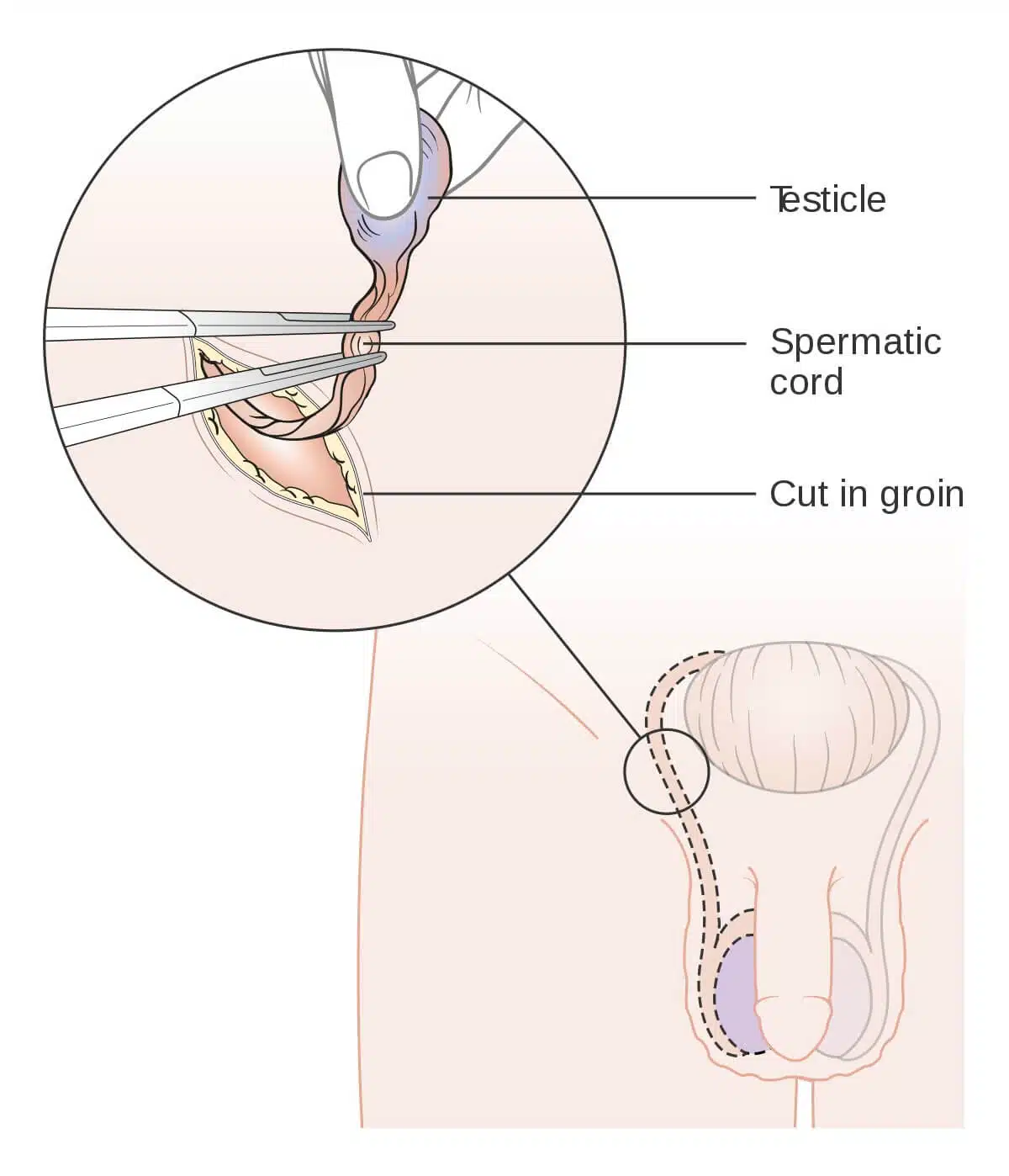
- Incision: The surgeon maketts a small incision in the groin or lower abdomen on the side of the undescended testicle. The location of the incision depends on the specific condition of the undescended testicle.
- Exploration and mobilization: The surgeon carefully explore the area to locate the undescended testicle. If the testicle is in the abdomen, it is gently moved, separating it from the surrounding tissues, blood vessels, and spermatic cord. The spermatic cords contain the blood vessels and nerves that supply the testicles.
- Pathway Creation: If the testicle is in the abdomen, the surgeon will create a passage (called the “neonatal testicular passage”) to move the testicle into the scrotum. This pathway allows the testicles to reach the scrotum without stressing the blood vessels and spermatic cord.
- Descending the Testicle: Once the path is in place, the surgeon will guide the testicle through the inguinal canal (if present) or along the newly created line and into the scrotum.
- Fixation: In some cases, to prevent the testicle from retracting into the abdomen, the surgeon may immobilize the testicle in its new position with sutures or small dissolvable stitches. Close the door: Once the testicle is well positioned in the scrotum, the surgeon closes the incision with sutures or stitches. In some cases, surgical glue may be used in place of traditional stitches.
- Closure: After the surgery, the child was taken to the recovery area, where he was closely monitored until he woke up from anesthesia. Most children are able to go home the same day of surgery or after a short follow-up period.
What is happening before Orchiopexy surgery?
Pre-operation instructions must be followed before the surgery. These often include:
- no eating for a time before surgery
- no drinking for a time before surgery
If arranged medicine to take the day off, you are supposed to take them with a minor sip of water. Also, depending on the age of the child or adult, food and water orders will differ. Patients organizing for orchiopexy must not eat or drink the night or midnight before surgery.
What happens during orchiopexy?
During the surgery, you will not sense pain or be conscious because general anesthesia is considered. The testicle is inspected and then located into the scrotum. The doctor
- creates a minor incision in the groin
- localize the testicle to be fixed
Is orchiopexy a major surgery?
No, orchiopexy is not considered a major surgical procedure. It can be performed on an outpatient basis, meaning you do not need to spend the night at the hospital. After the procedure, you are free to go home. Thus, do not be stressed out! Orchidopexy will not be risky.
Types of orchiopexy
From a technical point of view, this method is done in different approaches, which we briefly explain below:
- Inguinal orchiopexy: Inguinal orchiopexy approach also known open orchiopexy, involves shifting the testicle from the groin to the scrotum using a small incision.
- Abdominal orchiopexy (laparoscopic orchiopexy): on the other hand, utilizes laparoscopic surgery to move the testicle from the abdomen to the scrotum.
- Fowler-Stephens orchiopexy: the testicular blood vessels are separated and the testicle is relocated to the scrotum through a microsurgical technique. There are two main stages in Fowler-Stephens orchiopexy: First Step: The blood flow to the undescended testicle is cut off, which decreases the blood supply and makes the testicle more sensitive to lack of blood flow. Interval: A period of waiting is necessary for the testicle to decrease in size and adjust to the reduced blood flow. Second Step: The testicle is moved and fixed in the scrotum using surgical methods. A fresh blood supply is created by connecting the testicle to a different blood vessel.
- Two-step Fowler-Stephens: Two-step Fowler-Stephens surgery is similar to conventional Fowler-Stevens orchidopexy in that the procedure is performed in two steps, but the blood supply is controlled differently. The purpose of this modification is to increase the surgical success rate and minimize possible complications. The details of surgery may vary depending on the skill of the surgeon and the individual case of the patient.
- Two-stage orchiopexy: the testicle is initially secured in the groin and later moved to the scrotum after a few months.
Orchiopexy in adults
Commonly, orchiopexy is done in pediatric cases and according to USA National Institutes of Health (NIH), the most reliable evidence suggests that it is best to perform orchiopexy when a child is between 6 and 12 months old. Orchiopexy also can be performed in adults and teenagers. As you know, adults are people who are over 18 years old. And people under this age are called teenagers and children. Accordingly, and there are some indications for this process in adults:
- Improving Fertility: Undescended testicles can negatively impact fertility by affecting the production of sperm. Orchiopexy aims to enhance fertility by relocating the testicle(s) to the scrotum, which provides the optimal temperature for sperm production.
- Enhancing Comfort and Functionality: Undescended testicles can cause discomfort, pain, or awkwardness, especially during physical activities. By undergoing orchiopexy, these symptoms can be alleviated, resulting in improved overall functioning of the testicle.
- Lowering Cancer Risk: Adults with undescended testicles face a higher risk of developing testicular cancer. Orchiopexy can reduce this risk by placing the testicle(s) in the scrotum, enabling easier monitoring for any potential abnormalities.
Orchiopexy and infertility
Orchidopexy aims to improve fertility by repositioning the testicles, but its effectiveness is controversial. Studies show that early surgery may reduce the risk of testicular atrophy and impaired sperm production and improve fertility. However, complications such as nerve and blood vessel damage during surgery can affect fertility. Orchiopexy is generally considered beneficial in correcting cryptorchidism and possibly preserving fertility, but individual factors and surgical technique play an important role. In order to make an informed decision, it is essential to consult a doctor. Generally, we can say orchiopexy cannot cause infertility but you have to consult with fertility experts if you have done orchiopexy. Here, in TebMedTourism, best IVF clinic in the world, we are at your service to take you some advices about this issue.
Orchiopexy Cost
The cost of orchiopexy may vary widely depending on the country, clinic, and currency. It’s so expensive in some country such as USA and raise up to 12000 dollars. Orchiopexy cost in TebMedTourism, the best fertility related treatment clinic in Iran, is just about 900-1200 dollars. The quality of TebMedTourism is approved for all patients because of our expertise and experiences. For example, most of our urologist and surgon, embryologist are graduates from the best universities and hospitals in the world.
Complications of orchiopexy
As you know now, orchiopexy is a surgical procedure that is generally safe and effective in treating undescended testicles. However, like any surgery, it does come with potential risks and complications. It is important to note that these complications are relatively rare, and most people have successful outcomes from orchiopexy. Here we want explain you most orchiopexy side effects:
- Infection: One possible complication is infection at the surgical site. Signs of infection may include increased pain, redness, swelling, warmth, or discharge from the incision site.
- Bleeding: Another potential risk is excessive bleeding during or after the procedure, which can lead to the formation of a hematoma (a collection of blood) at the surgical site.
- Scarring: Scarring is a common result of any surgery, including orchiopexy. While the scars are usually small and hidden, some individuals may develop more noticeable scars.
- Recurrence: In some cases, the undescended testicle may reascend after orchiopexy, necessitating further treatment.
- Testicular atrophy: Rarely, there may be a decrease in the size of the testicle following orchiopexy, known as testicular atrophy. This risk is higher in cases where the testicle has remained undescended for a long time.
- Hydrocele: Fluid accumulation around the testicle, called a hydrocele, can occur as a result of the surgery. In most cases, this resolves on its own but may require further treatment in some instances.
- Anesthesia risks: Anesthesia risks also exist, including allergic reactions, adverse effects, and complications related to being under anesthesia.
- Spermatic Cord Injury: In rare instances, the spermatic cord, which contains blood vessels and the vas deferens, may be injured during the procedure, potentially impacting blood supply and fertility.
- Hernia: There is a slight risk of developing an inguinal hernia at the incision site.
- Pain: Finally, some individuals may experience ongoing pain or discomfort in the scrotal area after the surgery.
It is important to emphasize that the likelihood of experiencing complications is generally low, and most people undergo orchiopexy without significant issues. Surgeons take precautions to minimize these risks, and patients are closely monitored during the recovery period. If you or someone you know is considering orchiopexy, it is crucial to consult with a qualified healthcare provider, who can provide personalized guidance based on individual circumstances.
Orchiopexy complications later in life
Moreover, some complications might be occurred in long time after orchiopexy surgery. It should note that some of these complications may occur after orchiopexy soon and due to that, we will not explain them much here. So, here we want to describe you some main long-term side effects of orchiopexy:
- Testicular Atrophy: Testicular atrophy is one of the main post-orchiopexy problems. In this phenomenon testicles can decrease in size over time, either one or both. This can happen if the undescended testicle was not working properly or had poor blood flow before the orchiopexy procedure. Testicular atrophy or small testicle can also be caused by surgical trauma or complications.
- Decreased Fertility: While orchiopexy aims to improve fertility, it is possible that fertility may not be fully restored, especially if the surgery was done after puberty. Sperm production may improve but might not reach normal levels if the testicle’s function was compromised for a long time.
- Testicular Pain or Discomfort: Some people may experience pain or discomfort in the testicles years after the surgery. This could be due to the formation of scar tissue, nerve irritation, or other factors.
- Formation of Scar Tissue: Scarring is a normal part of the healing process after surgery, but excessive scar tissue can cause discomfort, pain, or a sensation of pulling.
- Reascent or Recurrence: In rare cases, an undescended testicle may move back up into the inguinal canal or abdomen after a successful orchiopexy.
- Hydrocele: Fluid buildup around the testicle (hydrocele) can occur as a delayed complication.
- Hernia: Inguinal hernias can develop at the site of the surgical incision, though this is uncommon.
It’s important to note that these complications do not always occur and are relatively rare. Most people who undergo orchiopexy have successful outcomes without long-term complications. Regular follow-up appointments with a healthcare provider can help monitor the health of the testicles and address any concerns that may arise later in life. If you have previously had orchiopexy and are experiencing new symptoms or concerns related to the surgical area or your testicles, it is recommended to consult a qualified healthcare provider or urologist for a proper evaluation and guidance. We are at TebMedTourism, provide you a free consultation in your fertility related injury!
Recovery after orchiopexy
Although there are some differences between recovery in children and adults, you should expect some points after orchiopexy; It is typical to experience swelling and bruising in the sac of the scrotum. These symptoms may worsen initially, but they will gradually improve over the course of the next month. It is common to observe a slight amount of bleeding from the incisions located in the lower abdomen and scrotum during the first couple of days. Here we want to tell you, how to recover after orchiopexy? So, let’s go know about it!
Recovery after orchiopexy in children
After an orchiopexy, most children often experience fatigue and may need extra sleep for the following two to three days to aid in their recovery. For children aged 12 months or older, they can typically resume their regular activities within two to three days of the surgery.
However, it is crucial for them to avoid any activities that may strain their abdominal or groin area. These activities may include tumbling, jumping, sprinting, lying on their stomach, and straddling toys such as a rocking horse, see-saw, swing, or tricycle. To prevent infection, it is essential to keep the affected areas clean. Before handling your child’s bandages and incision areas, remember to wash your hands thoroughly with soap and water.
While showering or sponge bathing your child is acceptable, it is advisable to avoid bathing them in a bathtub for approximately a week. It is important to note that every child’s recovery process is unique, and the time it takes may vary. Follow the instructions provided by your healthcare provider to effectively manage your child’s pain and discomfort.
Recovery after orchiopexy in adults
The recovery after orchiopexy for adults involves several stages aimed at ensuring healing, reducing discomfort, and restoring normal activities. The specific timeline may vary based on factors such as tthe surgical technique and individual health. After the surgery, which is typically done as an outpatient procedure, immediate recovery involves managing pain and swelling.
It is important for patients to rest and gradually increase their activity levels to prevent blood clots. Proper care of the incision site dressings is necessary for optimal healing. During the first week, pain and discomfort decrease, allowing patients to cautiously increase their activity levels. Follow-up appointments will monitor the healing of the incision, and orchiopexy stitches or sutures may be removed. As time goes on, swelling continues to decrease, enabling patients to gradually return to their normal routines while avoiding strain on the surgical area. If fertility concerns are present, semen analysis may be conducted to assess sperm quality. Long-term recovery involves ongoing follow-up appointments to track progress and address any concerns. Over time, the scar from the incision will fade.
Although this recovery timeline provides general guidance, individual experiences may vary. If severe pain, swelling, fever, or signs of infection occur, immediate medical attention should be sought. Ultimately, recovery from orchiopexy is a comprehensive process that requires adherence to medical instructions, close communication with healthcare providers, and patience as the body heals. By carefully following post-operative guidance and promptly seeking medical attention, when necessary, individuals can facilitate a successful and smooth recovery after orchiopexy.
What to do after orchiopexy surgery?
The following instructions are general guidelines. They may vary for your child but you can make free consultation with our experts in TebMedTourism for asking instruction, which specified for your child.
Generally, orchiopexy post operative care instructions can divide into three category, immediate post-operation, first few days, first week to several weeks, and also long-term instructions.
Immediate Post-Operative Period
- Rest and Recovery: Give yourself time to relax and recover right after your surgery. Feeling tired or groggy due to anesthesia is completely normal.
- Pain Management: Follow your healthcare provider’s instructions on taking prescribed pain medications to help with any discomfort. They may also recommend over-the-counter pain relievers.
- Incision Care: Keep the incision area clean and dry to avoid infections. Make sure to follow your healthcare provider’s advice on how to take care of the wound.
- Dressing and Bandages: If there is a dressing or bandage covering the incision, follow the provided guidelines on when and how to change it.
- Hydration and Nutrition: Stay properly hydrated and nourished to aid in the healing process. Eat a well-balanced diet that includes vitamins, minerals, and protein. Include foods that assist in tissue repair and boost your immune system.
First few days
- Activity limitations: To prevent strain on the surgical site, refrain from engaging in strenuous activities, heavy lifting, and vigorous exercise during the initial week.
- Diet and Hydration: Maintain a nutritious diet and ensure adequate hydration to promote healing and overall health.
- Pain and swelling: Follow your healthcare professional’s advice on using ice packs to minimize swelling and alleviate any pain or discomfort.
- Medication: Adhere to the prescribed antibiotic regimen to prevent infection. Take pain medication as necessary.
First Week to Several Weeks
- Gradual Increase in Activity: Follow your healthcare provider’s advice and slowly enhance your activity level. It is typically recommended to engage in light walking to improve blood circulation and reduce the risk of blood clots.
- Monitoring the Incision: Keep a close eye on the incision area for any signs of infection, such as heightened redness, swelling, warmth, or discharge. If you notice any worrisome changes, contact your healthcare provider immediately.
- Follow-Up Appointments: Make sure to attend all scheduled follow-up appointments to ensure proper healing and track your recovery progress.
Long-term
- Scar Care: Once the incision is fully healed, you can consider using silicone gel sheets or creams to minimize scarring.
- Physical Activity: Gradually resume regular physical activities, including exercise, sports, and other hobbies, as advised by your healthcare provider.
- Testicular Self-Exams: Continue performing regular testicular self-exams to monitor for any changes or abnormalities. We will describe how to do testicular self-exams at home
Testicular Self-Exams at Home
Regularly examining your testicles is crucial for maintaining your reproductive health. By conducting this simple self-exam at home, you can identify any changes or abnormalities. Here’s we describe how to do testicular self-exams at home step by step:
- Choose a Convenient Time: Select a time without interruptions when you can comfortably perform the self-exam. Many find it helpful to do it after bathing or showering, as the scrotal skin is relaxed.
- Stand in Front of a Mirror: Begin by standing in front of a mirror. Observe your scrotum for any visible alterations in size, shape, or skin texture. It’s normal for one testicle to appear slightly larger or hang lower than the other.
- Support Your Penis: Use one hand to gently lift your penis out of the way, exposing the testicles.
- Inspect One Testicle at a Time: Hold one testicle between your fingers and thumb of the other hand. Roll it gently between your fingers, checking for any lumps, bumps, or hard masses. You will feel an epididymis, a cord-like structure, on the top of each testicle. This is a normal part of the anatomy and not a lump.
- Be Thorough: While rolling the testicle between your fingers, ensure you cover its entire surface, including the front, sides, and back. Take your time and handle it gently.
- Pay Attention to Sensations: While examining each testicle, be alert to any sensations such as pain, discomfort, or heaviness
- Take Note of Any Changes: If you observe any changes such as new lumps, swelling, pain, or unusual sensations, make a record of it.
- Repeat for the Other Testicle: After completing the examination for one testicle, move on to the other one using the same gentle rolling motion.
- Perform Regular Self-Exams: Repeat this self-exam once a month to familiarize yourself with the normal texture of your testicles and detect any changes early on.
- Consult a Healthcare Professional: If you discover any unusual changes during your self-exam, get in touch with a healthcare provider for further evaluation. Not all changes are cancerous, but seeking professional advice is important.
Testicular growth after orchiopexy
After undergoing orchiopexy, a procedure to correct an undescended testicle, the growth and development of the testicle can change depending on a number of factors. Key considerations include age at surgery, success of the procedure, and personal health factors.
The ideal time for orchiopexy is usually before puberty, allowing the testicles to develop optimally. By inserting the testicle(s) into the scrotum, orchiopexy creates an environment for normal growth and development. This alteration can positively affect the growth trajectory and function of the testicles. In some cases, successful orchiopexy can lead to “catch-up growth,” in which one undescended testicle undergoes rapid growth to match the size of the other. However, individual variation plays an important role, influenced by genetics, hormonal factors and overall health.
It is important to note that although orchiopexy is intended to improve fertility, achieving this goal may involve factors beyond simple testicular development. Successful reproductive outcomes can also depend on early intervention and overall health. Postoperative follow-up is important to assess testicular growth and development over time.
Regular medical checkups provide insight into progress and help guide expectations It is essential to understand that testicular development is a gradual process. Direct comparison of previous undescended testicle growth with that of the other may not accurately reflect the natural rate of development, as individual responses may vary. In summary, testicular development after orchiectomy is influenced by age at surgery, success of the procedure, genetics, hormones, and individual variability. Although Orchidopexy provides an enhanced environment for development, individual results have varied.
Early intervention and ongoing medical monitoring contribute to the best possible outcome. If you are concerned about testicular growth after orchiopexy, consult a qualified health care professional or urologist who can provide you with information tailored to your particular situation.
Can an orchiopexy fail?
In general, in children under 2 years of age, the failure rate of orchiopexy is about 1.9%, and in children older than this age, it is 3%. This research shows that in general the rate of failure in orchiopexy is very low, but in some circumstances this may happen. Some of the factors that may contribute to the potential failure of orchids are bilateral activity and age at the time of primary activity. Failure to achieve satisfactory scrotal position (and testicular loss) after orchidectomy has been considered a potential surgical criterion for rehabilitation by pediatric surgeons.
What is the CPT code for orchiopexy related surgery?
According to the American Medical Association (AMA), The use of Current Procedural Terminology (CPT®) codes promotes consistent naming conventions for coding medical procedures and services. These codes play a crucial role in enhancing reporting accuracy and efficiency, as well as facilitating administrative tasks such as claims processing and the creation of medical care review guidelines. The CPT code for Orchiopexy, inguinal approach, with or without hernia repair is 5460. Also, CPT code for laparoscopic orchiopexy is 54690. For orchiopexy for testicular torsion, use CPT code 54600 (Testicular torsion reduction, surgery, with or without fixation of the contralateral testicle) or 54620 (Fixation of contralateral testis).
What is the ICD code for orchiopexy related surgery?
The US CDC states that: The International Classification of Diseases (ICD) is designed to promote international comparability in the collection, processing, classification, and presentation of mortality statistics. So, ICD code doesn’t use for surgical procedure such as orchiopexy but it uses for diseases.
What is the difference between orchidopexy and orchidectomy?
Orchidopexy and orchidectomy are two distinct surgical procedures involving the testicles, but they serve different purposes and are performed under different circumstances.Orchiectomy is the surgical procedure to remove one or both testicles and it has different prospective to orchiopexy. Important notes about orchiectomy are written below:
- For testicular cancer, removal of the cancerous or potentially cancerous testicle is common.
- It can also be used to treat certain conditions, such as hormone-sensitive prostate cancer, where testosterone production decreases when the testicles are removed.
- Orchiectomy causes permanent infertility because it removes the sperm-producing source and testosterone.
Radical orchiectomy
A radical orchiectomy is a surgical operation that entails the total extraction of one or both testicles. It is commonly performed to treat testicular cancer or other medical conditions necessitating testicle removal. The procedure is regarded as radical because it entails removing the entire testicle, encompassing the spermatic cord and adjacent tissues.
Can bilateral orchiopexy cause infertility?
Bilateral orchiopexy can lead to an incidence of infertility as high as 59%, and up to 32% of men with Unilateral cryptorchidism can be infertile despite surgical correction with testicle fixation.