Abortion is a medical procedure that ends a pregnancy. While it is generally safe when performed by professionals, some women worry about its effect on future fertility. In most cases, a properly done abortion does not cause infertility. However, complications like infections, uterine scarring, or hormonal imbalances can sometimes make it harder to get pregnant later, leading to concerns about infertility after abortion.
In this article, we will explain how abortion affects fertility, the possible risks, and ways to improve reproductive health after an abortion. Understanding these factors can help women make informed decisions and care for their fertility.
Understanding the Link Between Abortion and Infertility
Abortion is a common medical procedure, but many women wonder if it affects their ability to get pregnant in the future. The good news is that, in most cases, abortion does not directly lead to infertility. When appropriately performed by a skilled healthcare provider, it typically does not cause long-term issues with fertility.
However, there are some exceptions. If there are complications, such as infections or damage to the uterus, these can potentially affect future pregnancies. In some cases, concerns about infertility after abortion arise when these complications lead to difficulties in conceiving. The risk of these complications is relatively low, especially when the procedure is done in a clean, medical environment with proper care.
It’s important to understand that infertility is usually caused by a variety of factors, and an abortion is just one part of the bigger picture. Many women who have had abortions go on to have healthy pregnancies later without any problems. Understanding how abortion might affect fertility helps women make better decisions and take steps to protect their reproductive health.

Common Causes of Infertility Post-Abortion
While most women can conceive again after an abortion without any issues, there are a few situations where fertility can be affected. Here are some of the most common causes of infertility that may occur after an abortion:
Infections:
Infections that occur during or after the abortion can lead to pelvic inflammatory disease (PID), a condition where the reproductive organs, like the uterus and fallopian tubes, become inflamed. PID can cause scarring and blockages, which might make it more difficult for an egg to travel through the fallopian tubes, potentially leading to infertility.
Uterine Scarring (Asherman’s Syndrome):
Sometimes, during an abortion, the lining of the uterus can be injured, leading to scarring. This scarring can make it harder for an embryo to implant properly or, in severe cases, prevent pregnancy altogether. This condition is known as Asherman’s syndrome and is rare but treatable.
Hormonal Imbalances:
After an abortion, some women may experience hormonal changes. These changes can affect ovulation (the release of eggs) and the regularity of menstrual cycles. If ovulation is disrupted, it may be harder to get pregnant. However, in most cases, hormone levels balance out over time, allowing fertility to return.
Cervical Damage:
In rare cases, an abortion can cause damage to the cervix, which can affect the ability to carry a pregnancy to term. If the cervix is weakened or shortened, it may not stay closed during pregnancy, which can lead to early miscarriage or premature birth.
Most of these conditions are treatable, and many women have successful pregnancies after receiving medical care. The key is to monitor your health and seek professional advice if you have concerns about your fertility after an abortion.
Medical vs. Surgical Abortion: Impacts on Future Fertility
When it comes to abortion, there are two main types: medical abortion and surgical abortion. Both procedures are generally safe when performed under the right conditions, but they can have different effects on a woman’s future fertility.
Medical Abortion:
A medical abortion involves taking medication to end the pregnancy. This is usually done in the early weeks of pregnancy (up to 10 weeks). The most common medications used are mifepristone and misoprostol.
Since medical abortion doesn’t involve any surgical instruments, it is generally considered to have a lower risk of causing scarring or physical injury to the uterus. As a result, it typically has fewer long-term effects on fertility. Most women who undergo a medical abortion can get pregnant again in the future without any issues.
However, like any medical procedure, there can still be complications, such as infection or incomplete abortion. If these issues are not properly addressed, they could affect fertility, though this is rare.
Surgical Abortion:
A surgical abortion, often referred to as aspiration or dilation and curettage (D&C), involves a doctor using instruments to remove the pregnancy from the uterus. This method is typically performed later in the first trimester or more complicated cases.
Surgical abortion carries a slightly higher risk of complications compared to medical abortion, such as infections or injury to the uterus or cervix. In some cases, damage to the uterine lining or scarring may occur, which could make future pregnancies more difficult. However, these complications are rare, and most women recover without any long-term effects.
In general, both types of abortion are safe, and fertility is usually not impacted in the long term. The risk of complications can be minimized by ensuring the procedure is done by a qualified professional in a safe medical environment. After either type of abortion, most women can expect their fertility to return to normal relatively quickly.
Recognizing Symptoms of Infertility After an Abortion
After an abortion, most women regain their fertility quickly and can conceive without complications. However, in some cases, infertility may occur due to underlying issues like infections, uterine scarring, or hormonal imbalances. Recognizing the symptoms of infertility early can help women seek timely medical intervention and improve their chances of conceiving in the future.
- Irregular or Absent Menstrual Cycles: One of the first signs of infertility after an abortion is irregular or absent periods. If your menstrual cycle becomes unpredictable, too short, too long, or disappears altogether, it may indicate problems with ovulation. Hormonal imbalances caused by stress, changes in body weight, or underlying reproductive issues may contribute to these changes.
- Severe Menstrual Pain or Heavy Bleeding: While some cramping and bleeding are normal after an abortion, persistent and severe pain during menstruation may signal a problem. Conditions like Asherman’s syndrome (uterine scarring) or infections can lead to painful periods and difficulty getting pregnant. Heavy bleeding or blood clots could also indicate issues with the uterine lining.
- Pelvic Pain and Discomfort: Chronic pelvic pain, especially outside of menstruation, may be a sign of pelvic inflammatory disease (PID) or uterine scarring. PID can result from untreated infections after an abortion and may lead to blocked fallopian tubes, making conception difficult. Women experiencing persistent pain should consult a doctor for evaluation.
- Difficulty Getting Pregnant: If you have been trying to conceive for more than a year (or six months if over 35) without success, it may indicate infertility. Abortion itself is not a direct cause of infertility, but if complications like uterine damage or infections occur, they could make conception more challenging. A fertility specialist can help determine the cause and recommend treatments.
- Abnormal Vaginal Discharge: Unusual vaginal discharge with a foul smell, yellow or green color, or a thick consistency may indicate an infection. Infections that spread to the reproductive organs can lead to fallopian tube blockages, which prevent sperm from meeting the egg. Treating infections early can help prevent long-term fertility problems.
- Pain During Intercourse: Experiencing pain during intercourse after an abortion may suggest underlying reproductive health issues. Conditions like uterine scarring, pelvic infections, or cervical damage can contribute to discomfort and impact fertility. If pain persists, seeking medical evaluation is important.
If you experience any of these symptoms, it is important to seek medical advice. A doctor can perform tests such as ultrasounds, hormone evaluations, or hysteroscopy (a procedure to examine the uterus) to identify any fertility-related concerns. Early diagnosis and treatment can help restore reproductive health and improve the chances of conception.
Treatment Options for Infertility Resulting from Abortion Complications
Experiencing infertility after an abortion can be emotionally and physically challenging. In many cases, medical treatment can help restore fertility and improve the chances of conception. The right approach depends on the underlying cause, such as infections, uterine scarring, hormonal imbalances, or structural damage to the reproductive organs. Below are the most effective treatment options available for infertility resulting from abortion complications.
Treating Infections and Pelvic Inflammatory Disease (PID)
If an infection after an abortion has led to pelvic inflammatory disease (PID), early treatment with antibiotics is crucial. Mild infections can often be managed with oral antibiotics, while severe cases may require intravenous antibiotics or hospitalization. If PID has caused scarring or blocked fallopian tubes, surgery may be needed to remove the scar tissue and restore normal function.
Surgical Treatment for Uterine Scarring (Asherman’s Syndrome)
Uterine scarring, also known as Asherman’s syndrome, can prevent an embryo from implanting or cause recurrent miscarriages. Treatment involves a minor surgical procedure called hysteroscopic adhesiolysis, where a doctor uses a small camera and surgical tools to remove scar tissue inside the uterus. After surgery, hormone therapy or an intrauterine device (IUD) may be used temporarily to help the uterine lining heal properly.
Hormonal Therapy for Ovulation Disorders
Hormonal imbalances after an abortion can affect ovulation, leading to irregular or absent menstrual cycles. Treatment options may include:
- Oral medications like Clomiphene citrate (Clomid): stimulate ovulation in women with irregular cycles.
- Hormone replacement therapy (HRT): Helps restore normal estrogen and progesterone levels.
- Lifestyle modifications: Maintaining a healthy weight, reducing stress, and eating a balanced diet can help regulate hormones naturally.
Fertility Treatments for Blocked Fallopian Tubes
If an abortion-related infection has led to blocked fallopian tubes, conception may be difficult. Depending on the severity, doctors may recommend:
- Laparoscopic surgery: a minimally invasive procedure to remove scar tissue and open the fallopian tubes.
- In vitro fertilization (IVF): IVF in Iran is of interest to many foreign patients. If the damage is severe, IVF bypasses the fallopian tubes entirely by fertilizing the egg in a lab and transferring the embryo directly into the uterus.
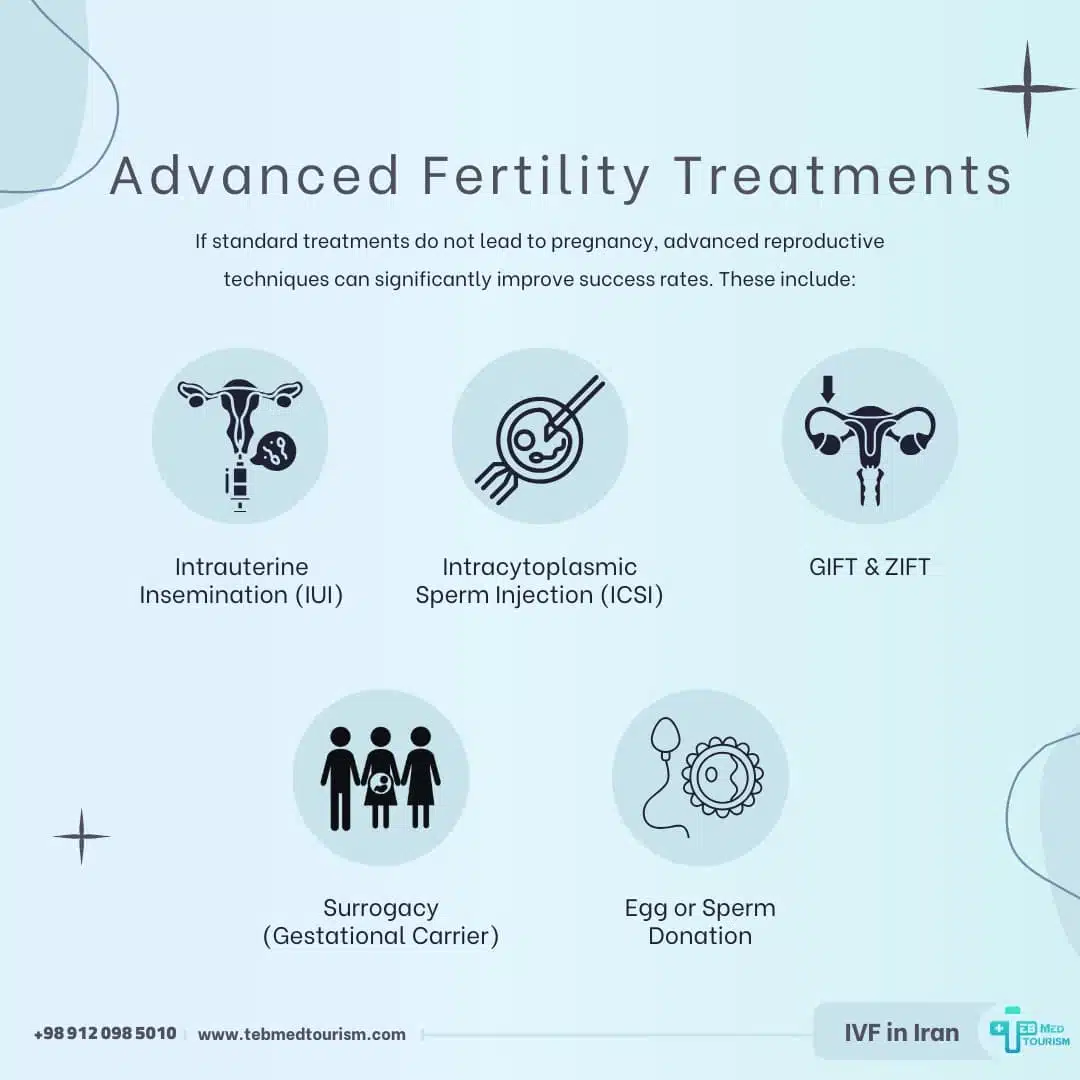
Advanced Fertility Treatments
If standard treatments do not lead to pregnancy, advanced reproductive techniques can significantly improve success rates. These include:
Intrauterine Insemination (IUI)
It is a simple procedure where sperm is directly placed into the uterus around the time of ovulation to increase the chances of fertilization. This is useful for mild infertility cases related to ovulation disorders or mild male factor infertility.
Intracytoplasmic Sperm Injection (ICSI)
ICSI in Iran is performed with the best quality. A specialized IVF technique where a single sperm is injected directly into an egg to improve fertilization, especially in cases of male infertility or poor sperm quality.
Gamete Intrafallopian Transfer (GIFT) & Zygote Intrafallopian Transfer (ZIFT)
- GIFT: Sperm and eggs are mixed and placed directly into the fallopian tube, allowing fertilization to occur naturally inside the body.
- ZIFT: The egg is fertilized in the lab, and the zygote (early embryo) is then transferred into the fallopian tube instead of the uterus.
These methods are less common today due to the high success rates of IVF.
Surrogacy (Gestational Carrier)
Surrogacy in Iran is one of the ways to have a child after an abortion. If a woman is unable to carry a pregnancy due to uterine abnormalities, severe scarring, or recurrent pregnancy loss, gestational surrogacy is an option. A surrogate carries the intended parent’s embryo, created via IVF, until birth.
Egg or Sperm Donation
Egg donation in Iran is very common for the treatment of infertility. In addition, sperm donation in Iran is also performed for the treatment of infertility in men. For individuals with poor egg or sperm quality, donor eggs or sperm can be used in IVF to increase the chances of a successful pregnancy.
Cryopreservation (Egg, Sperm, or Embryo Freezing)
- Egg freezing (oocyte cryopreservation): Preserving eggs for future use.
- Sperm freezing: Common for men undergoing medical treatments that may affect fertility.
- Embryo freezing: Storing embryos created via IVF for later implantation.
Artificial Insemination
A fertility procedure where sperm is artificially placed into the reproductive tract, either in the uterus (IUI) or cervix, to assist conception.
Cervical Insufficiency Management
If cervical damage from an abortion has weakened the cervix, it may lead to pregnancy loss or premature birth. Treatment options include:
- Cervical cerclage: A surgical procedure where the cervix is stitched closed during pregnancy to prevent miscarriage.
- Progesterone therapy: Helps strengthen the cervix and reduce the risk of premature labor.
The Dangers of Unsafe Abortions and Their Impact on Fertility
In many countries, abortion remains highly restricted or even illegal, forcing women to seek unsafe procedures that put their health at serious risk.
The lack of access to safe medical care results in abortions being carried out in unhygienic conditions by untrained individuals, leading to life-threatening complications such as severe infections, hemorrhages, and permanent reproductive damage.
These dangers not only threaten women’s lives but also increase the risk of infertility after abortion, making future pregnancies difficult or even impossible.
Pakistan is one of the countries where unsafe abortions have become a significant public health issue. According to a Pulitzer Center report, an estimated 2.25 million abortions are performed annually in Pakistan, often under unsafe conditions.
Due to strict legal restrictions and social stigma, many women undergo procedures without proper medical supervision.
This lack of post-abortion care increases the risk of pelvic infections, uterine scarring, and Asherman’s syndrome, a condition where scar tissue forms inside the uterus, making implantation of a fertilized egg difficult or impossible.
The fear of legal consequences prevents many women from seeking timely medical help, causing untreated infections and complications to escalate, sometimes leading to death.
However, Pakistan is not the only country where unsafe abortions pose a serious threat to women’s health. In El Salvador and Honduras, abortion is completely banned, even in cases of rape or when the mother’s life is at risk.
Women suspected of having an abortion can face imprisonment, forcing many to seek dangerous and unregulated procedures. In the Philippines, where abortion is illegal under all circumstances, thousands of women suffer complications due to unsafe terminations.
Many of these women die from untreated infections or excessive bleeding because they fear seeking medical attention. Countries with restrictive abortion laws often have higher maternal mortality rates, as women are left with no safe options when facing unwanted pregnancies.
Restrictive laws do not stop abortions from happening; they only push them into unsafe environments. The World Health Organization (WHO) has emphasized that access to safe abortion services and post-abortion care is essential to reducing maternal deaths and long-term reproductive health problems.
Ensuring that women have access to contraception, proper medical care, and reproductive health education can help prevent the need for unsafe procedures.
In many cases, when a qualified professional safely performs abortion, fertility remains unaffected. However, when performed in unsafe conditions, the risk of infections, uterine damage, and infertility increases significantly.
Addressing the global crisis of unsafe abortions requires more than just legal reforms. It requires better access to reproductive healthcare, comprehensive education, and the destigmatization of abortion-related medical services.
By improving healthcare systems and supporting women’s reproductive rights, the risks associated with unsafe abortions can be significantly reduced, helping to protect both the health and fertility of millions of women worldwide.
Can abortion cause infertility?
In most cases, abortion does not cause infertility when performed safely by a qualified medical professional. However, complications such as infections, uterine scarring (Asherman’s syndrome), and cervical damage can increase the risk of infertility after abortion. These complications are rare but more likely to occur in unsafe or unregulated procedures.
How soon can I get pregnant after an abortion?
Fertility can return as early as two weeks after an abortion, as ovulation resumes quickly. However, doctors usually recommend waiting until the menstrual cycle normalizes before trying to conceive. This allows the uterus to heal properly and reduces the risk of complications in future pregnancies.
What should I do if I have trouble getting pregnant after an abortion?
If you are struggling to conceive, consult a fertility specialist. They may recommend tests such as ultrasounds, hormone level assessments, or hysteroscopy to check for uterine scarring or other issues. Treatment options vary depending on the cause and may include hormone therapy, surgery to remove scar tissue, or assisted reproductive technologies like IVF.
Can infections after an abortion lead to infertility?
Yes, infections such as pelvic inflammatory disease (PID) can damage the fallopian tubes and uterus, leading to infertility. Signs of an infection include fever, severe abdominal pain, foul-smelling vaginal discharge, and prolonged bleeding. Seeking medical treatment early can prevent long-term damage.
Is infertility after abortion permanent?
Not always. Many causes of post-abortion infertility, such as hormonal imbalances or uterine scarring, can be treated successfully with medical or surgical interventions. Early diagnosis and proper treatment improve the chances of conceiving naturally.
How can I reduce the risk of infertility after an abortion?
Ensuring the procedure is performed by a qualified healthcare provider, following post-abortion care guidelines, and seeking prompt medical attention for any complications can help protect fertility. Practicing safe sex and using contraception can also prevent unintended pregnancies and reduce the need for repeat abortions.